Definition and differentiation: What is aplastic anaemia and how does it differ from other forms of anaemia and blood disorders?
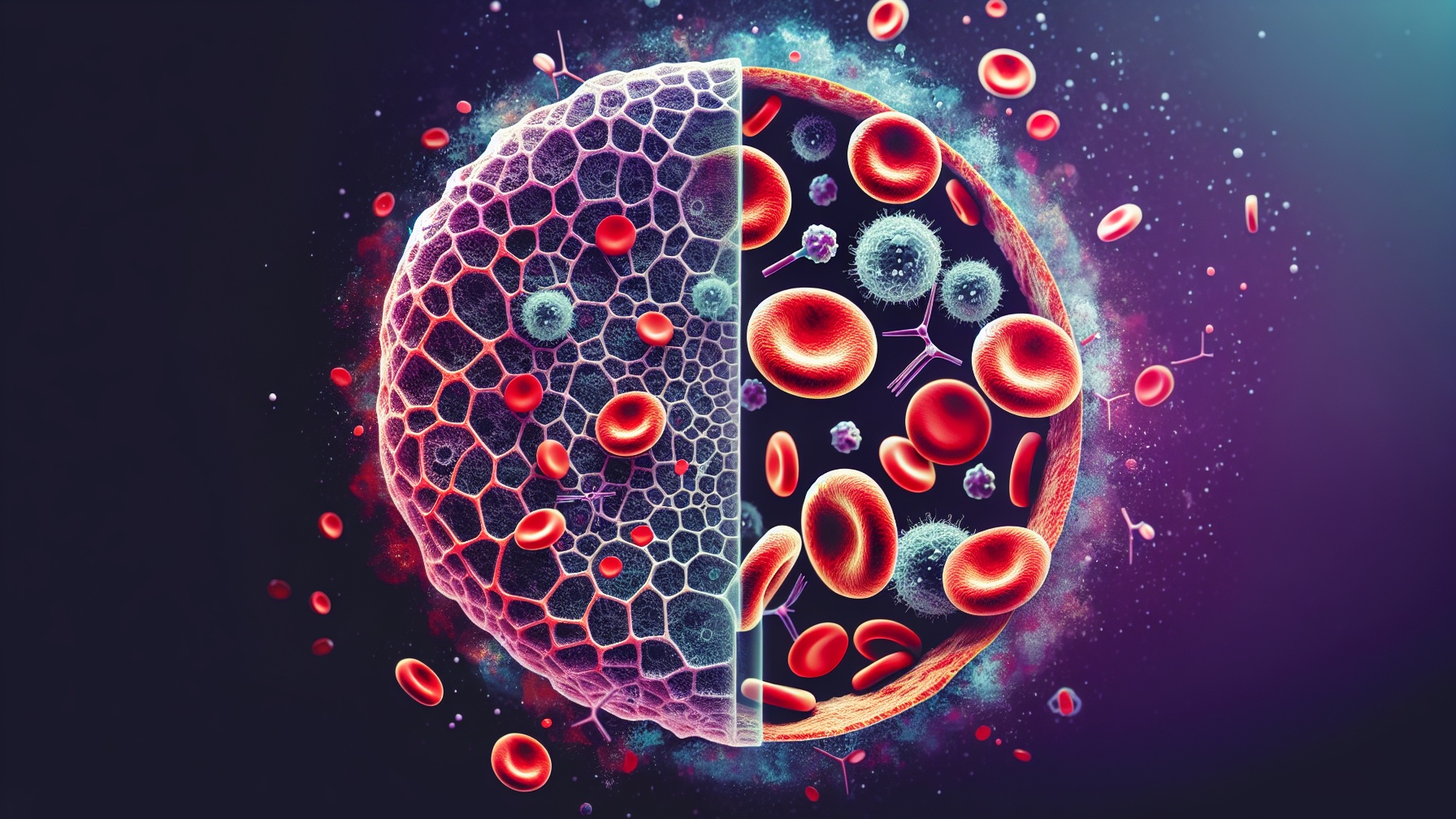
Aplastic anaemia is a rare but potentially life-threatening disease of the haematopoietic system characterised by pancytopenia. Pancytopenia means a reduction in all three cell series in the blood: erythrocytes (red blood cells), leucocytes (white blood cells) and thrombocytes (platelets). This reduction is the result of damage to or dysfunction of the bone marrow, the site of haematopoiesis. In contrast to other forms of anaemia, which are often due to a lack of specific nutrients such as iron (iron deficiency anaemia) or vitamin B12 (pernicious anaemia) and selectively affect only the erythrocytes, aplastic anaemia affects the production of all blood cells. It also differs from haemolytic anaemia, in which the red blood cells are broken down prematurely, and from myelodysplastic syndromes (MDS), which also affect the bone marrow but are often associated with abnormal cell maturation and an increased risk of transformation into acute leukaemia. In comparison to other blood diseases such as leukaemia or lymphoma, in which there is an uncontrolled proliferation of certain blood cells, the characteristic of aplastic anaemia is precisely the opposite: an ineffectiveness of the bone marrow to produce sufficient blood cells, which leads to a severe impairment of the immune defence, oxygen supply and blood clotting. Aplastic anaemia is therefore an independent and serious disorder of blood formation that differs fundamentally from other forms of anaemia and haematological diseases.
Causes and risk factors: What factors can trigger aplastic anaemia?
The causes and risk factors of aplastic anaemia are varied and can be both acquired and inherited, although in many cases the exact aetiology remains unclear (idiopathic aplastic anaemia). Acquired causes include certain medications, including some antibiotics (e.g. chloramphenicol), anticonvulsants (e.g. carbamazepine), non-steroidal anti-inflammatory drugs (NSAIDs) and chemotherapeutic agents. Certain chemicals such as benzene and other organic solvents, insecticides and pesticides can also damage the bone marrow and trigger aplastic anaemia. Viral infections, in particular parvovirus B19 (more common in children), hepatitis viruses (especially non-A, non-B, non-C hepatitis) and Epstein-Barr virus (EBV), are also discussed as possible triggers. Autoimmune reactions, in which the immune system mistakenly attacks the bone marrow, are an important cause, often in connection with T-cell-mediated processes. Less common are inherited forms of aplastic anaemia, such as Fanconi anaemia, a genetic disorder associated with an increased susceptibility to bone marrow failure and certain types of cancer. Other rare hereditary syndromes associated with aplastic anaemia include dyskeratosis congenita and Diamond-Blackfan syndrome. Exposure to high doses of ionising radiation (e.g. from accidents or radiotherapy) can also damage the bone marrow and lead to aplastic anaemia. Pregnancy can also trigger aplastic anaemia in rare cases.
Pathophysiology: Description of the mechanisms that lead to bone marrow damage and reduced haematopoiesis in aplastic anaemia.
The pathophysiology of aplastic anaemia is characterised by destruction or inactivation of the haematopoietic stem cells in the bone marrow, leading to pancytopenia, i.e. a deficiency in all three cell lines of the blood (erythrocytes, leukocytes and thrombocytes). The primary mechanism often involves a misdirected immune response in which autoreactive T cells attack and destroy the haematopoietic stem cells. This T cell-mediated cytotoxicity is amplified by the release of cytokines such as interferon-gamma (IFN-γ) and tumour necrosis factor-alpha (TNF-α), which induce stem cell apoptosis and inhibit proliferation of the remaining cells. In some patients, intrinsic stem cell deficiency also plays a role, for example due to mutations in genes responsible for DNA repair or telomere maintenance. Regardless of the initial cause, the damage to the stem cells leads to a reduction in the number of cells and a change in the bone marrow environment. The bone marrow, normally rich in haematopoietic cells, is replaced by fatty tissue (bone marrow aplasia), which additionally prevents the remaining stem cells from differentiating and multiplying. This loss of functional stem cells and the impaired bone marrow environment result in a significant reduction in haematopoiesis, which ultimately causes the clinical manifestations of aplastic anaemia.
Symptoms and clinical manifestations: What are the symptoms of aplastic anaemia?
Aplastic anaemia manifests itself clinically through a triad of symptoms that are attributable to pancytopenia, i.e. the lack of all three cell series of the blood (erythrocytes, leukocytes and thrombocytes). Anaemia, caused by the lack of red blood cells, primarily manifests itself in pronounced tiredness, weakness, paleness of the skin and mucous membranes and shortness of breath, especially during physical exertion. These symptoms can develop gradually and steadily worsen as the disease progresses. The lack of leukocytes, especially neutrophil granulocytes (neutropenia), leads to an increased susceptibility to infections, which can manifest themselves in the form of frequent and serious bacterial, viral or fungal infections. Typical clinical manifestations include fever of unknown origin, recurrent respiratory tract infections, skin infections and inflammation of the mouth and throat (mucositis). Thrombocytopenia, the lack of blood platelets, causes an increased tendency to bleed. This can manifest itself in the form of petechiae (punctiform skin haemorrhages), ecchymoses (extensive bruising), nosebleeds (epistaxis), bleeding gums (gingival bleeding), prolonged bleeding after injuries or operations and menorrhagia (increased menstrual bleeding) in women. In severe cases, spontaneous bleeding into internal organs, such as the gastrointestinal tract or the brain, can also occur, which can be life-threatening.
Diagnostics: What diagnostic procedures are used to detect aplastic anaemia?
The diagnosis of aplastic anaemia is a multi-stage process that aims not only to identify the disease, but also to determine its cause. It begins with a detailed medical history, during which the doctor asks about previous illnesses, medication (especially those associated with bone marrow damage), exposure to chemicals, radiotherapy and a family history of blood disorders. The subsequent physical examination serves to identify clinical signs such as pallor, petechiae (punctiform skin haemorrhages), ecchymoses (bruising) or signs of infection. A central element is the blood count, which shows pancytopenia, i.e. a reduction in all three cell series (erythrocytes, leucocytes, thrombocytes). However, pancytopenia alone is not specific for aplastic anaemia, which is why a bone marrow puncture and biopsy are essential. These procedures allow microscopic assessment of the bone marrow, which typically shows a lack of cells (hypocellularity) with an increased fat content. The histological examination also serves to exclude other causes of pancytopenia, such as myelodysplastic syndromes or infiltration of the bone marrow by tumour cells. Special tests are carried out to further narrow down the aetiology of aplastic anaemia. These include tests for paroxysmal nocturnal haemoglobinuria (PNH), a clonal disease that can be associated with aplastic anaemia, as well as tests for autoantibodies against bone marrow cells. Genetic tests may also be indicated to detect congenital forms of aplastic anaemia, such as Fanconi anaemia.
Treatment: Overview of the various treatment options for aplastic anaemia
The treatment of aplastic anaemia is primarily aimed at stabilising blood values, fighting infections and correcting the underlying bone marrow insufficiency. Supportive therapy, as the first pillar of treatment, includes regular transfusions of red blood cell and platelet concentrates to compensate for anaemia and bleeding tendencies and to improve the patient's quality of life. As patients with aplastic anaemia have an increased risk of infection, the early and aggressive use of antibiotics for bacterial infections is essential. Antimycotics and antivirals may also be indicated if necessary. A curative option is immunosuppressive therapy, which is primarily considered for patients who are not suitable for a bone marrow transplant or do not have a suitable donor. Antithymocyte globulin (ATG) and cyclosporine A are usually used to suppress the immune system and protect the remaining haematopoietic cells in the bone marrow from autoimmune attacks. Another curative option, which is often considered the treatment of choice, is allogeneic stem cell transplantation, in which healthy stem cells from a suitable donor replace the patient's insufficient bone marrow. However, this procedure is associated with risks, including graft-versus-host disease (GvHD), in which the transplanted cells attack the recipient's body, and requires intensive preparation and follow-up care.
Prognosis and progression: How does the prognosis of aplastic anaemia depend on the severity of the disease?
The prognosis and course of aplastic anaemia are significantly influenced by the severity of the disease, the age of the patient and the chosen therapy. In patients with severe aplastic anaemia, defined by a significant reduction in blood cells (granulocytes < 500/µl, platelets < 20,000/µl, reticulocytes < 1%), the untreated prognosis is poor, often with a median survival time of a few months. Spontaneous remissions are rare. The age of the patient plays an important role, as younger patients generally respond better to immunosuppressive therapy and tolerate bone marrow transplantation better. The treatment options have a considerable influence on the prognosis. Allogeneic stem cell transplantation from a suitable family donor offers the chance of a cure, especially for younger patients. However, it is associated with risks such as graft-versus-host disease (GvHD). Immunosuppressive therapy, usually with antithymocyte globulin (ATG) and cyclosporine A, can lead to an improvement in blood counts, but the response is not always complete and relapses are possible. Patients who respond to immunosuppressive therapy can achieve an acceptable quality of life in the long term, but there is a risk of clonal evolution to myelodysplastic syndromes (MDS) or acute myeloid leukaemia (AML).
Current research and future perspectives: What are the current research approaches to aplastic anaemia?
Current research is focusing intensively on gaining a deeper understanding of the pathophysiology of aplastic anaemia, in particular the role of the immune system and the dysregulation of T cells in the destruction of haematopoietic stem cells. A promising branch of research is investigating the significance of specific cytokines and signalling pathways involved in the autoimmune reaction with the aim of developing more targeted and less toxic immunosuppressants. Furthermore, the significance of genetic predispositions and acquired mutations, particularly in connection with clonal haematopoiesis of indeterminate potential (CHIP), is being investigated in order to better identify risk factors and enable personalised therapeutic approaches. In the field of therapy, the focus is on improving outcomes after allogeneic stem cell transplantation by optimising conditioning regimes, reducing graft-versus-host disease (GvHD) and improving the availability of suitable donors, for example through the use of haploidentical transplants. New immunomodulatory substances that selectively influence the immune system without suppressing the entire immune defence are also being tested. Research into gene and cell therapies, in particular CRISPR-based approaches to correct genetic defects in hereditary forms of aplastic anaemia, offers potentially curative options in the long term. Finally, improved diagnostic procedures are being developed, including sensitive methods for the early detection of bone marrow failure and the identification of specific immunological or genetic markers that enable a more precise prognosis and treatment planning.
Frequency therapy - nosode aplastic anaemia
Frequency therapy is an innovative approach that is becoming increasingly important in the treatment of aplastic anaemia. In this form of therapy, specific frequencies are used to activate the body's self-healing powers and promote balance in the haematopoietic system. Nosodes based on the principles of homeopathic medicine are used in frequency therapy. Nosodes are homeopathic remedies that are produced from pathologically altered tissues or secretions and are used to treat diseases by stimulating the body's own defence mechanisms. When used for aplastic anaemia, these frequencies aim to support the healthy function of the bone marrow and promote blood formation. Initial clinical studies show promising results in terms of an improvement in blood parameters and a reduction in symptoms associated with this severe disease. Nevertheless, it is important to consider this form of therapy as a complement to conventional treatment approaches and to work closely with the treating physician in order to achieve the best possible results.

