What is basal cell nevus syndrome?
Basal cell nevus syndrome (BCNS), which is also known as Gorlin syndrome or nevoid basal cell carcinoma syndrome (NBCCS) , is an autosomal dominant hereditary disease. Patients suffering from BCNS tend to develop various carcinomas. Among them multiple basal cell carcinomas (BCC), jaw cysts as well as skeletal anomalies/rib anomalies, thickening of the horny layer (hyperkeratosis) especially of the palms of the hands and soles of the feet, ectopic intracranial calcifications and shape abnormalities in the face (facial dysmorphia) frequently occur. Basal cell nevus syndrome ( ) is more common than average between the ages of 30 and 50.
What causes basal cell nevus syndrome?
Basal cell nevus syndrome is caused by mutations in the PTCH1 gene (chromosome 9) for the patched receptor. PTCH1 is a transmembrane protein that inhibits the SMO protein. If this is constantly activated, there is rapid tissue growth (cell proliferation). Basal cell nevus syndrome is inherited in an autosomal dominant manner .
How can basal cell nevus syndrome be detected early?
First-degree relatives of patients with basal cell nevus syndrome should be tested for the gene mutation in PTCH1 at an early stage in order to detect a disease at an early stage if necessary.
What are the symptoms of basal cell nevus syndrome?
Patients, who suffer from basal cell nevus syndrome, usually develop pale to brownish pigmented nodules on their face at an early age. In addition, they usually have a facial shape with a protruding lower jaw and a forehead that is curved forward. In the jaw area, cysts can also originate from the teeth. Often there are also skeletal malformations, especially of the ribs and vertebrae, and hyperkeratosis of the palms and/or soles.
Also, the following neurological abnormalities may be indicative of a medulloblastoma , which is caused by basal cell nevus syndrome:
- Headache,
- Drowsiness, which may alternate with disturbances of consciousness,
- morning vomiting,
- Movement and/or coordination disorders,
- Tendency to fall.
People who observe these signs in themselves or their child should consult a doctor as soon as possible.
What diseases can develop from basal cell nevus syndrome?
The following clinical features may develop from basal cell nevus syndrome:
- early-appearing malignant skin tumours (basaliomas),
- Dimples that form on the inner surfaces of the hands and/or feet,
- Formation of jaw cysts,
- Development of benign tumours (fibromas) of the ovaries,
- conspicuous skull shapes,
- Calcification of the meninges,
- Development of rib and/or vertebral anomalies,
- fused fingers since birth,
- cataract,
- rather rarely, a brain tumour (medulloblastoma) occurs in infancy
How is basal cell nevus syndrome diagnosed?
The BCNS is divided into main and secondary criteria, which play an important role in the diagnosis. If two main criteria and one secondary criterion or one main criterion with three secondary criteria are present, a clinical diagnosis of basal cell nevus syndrome can be made. The following factors make up the so-called major criteria:
- Presence of multiple basal cell carcinomas or the formation of a single basal cell carcinoma before the age of 30,
- Presence of odontogenic keratocysts of the jaws,
- palmar/plantar dimpling,
- Calcification of the cerebral crescent (falx cerebri),
- First-degree relative suffering from basal cell nevus syndrome
Ancillary criteria include:
- Presence of a medulloblastoma (malignant brain tumour) in childhood,
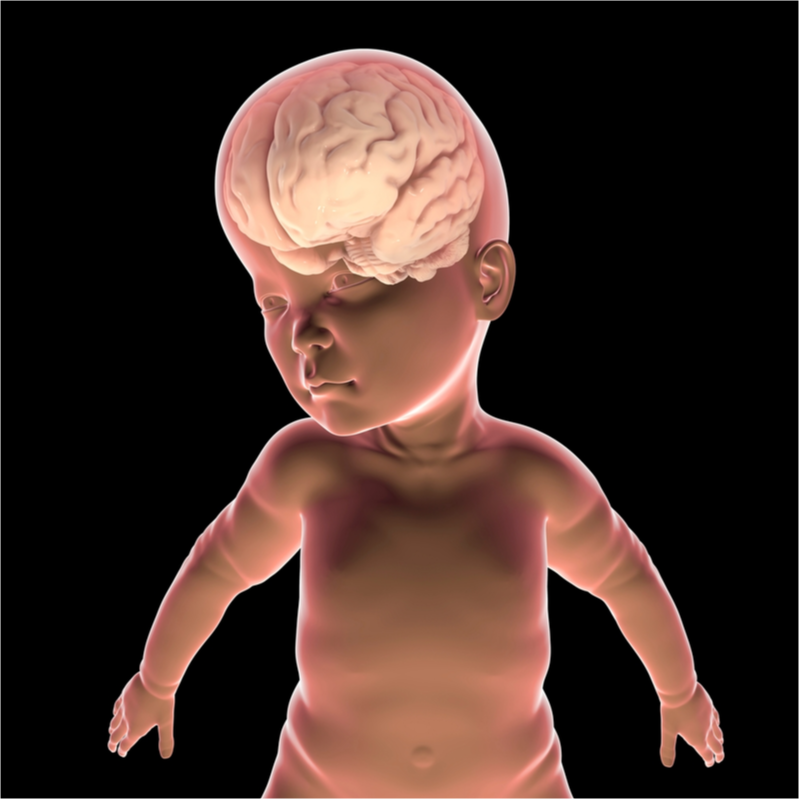
- large head (macrocephaly),
- Presence of cleft lip and palate,
- Anomalies of the vertebral bodies and/or ribs,
- preaxial or postaxial fused fingers or toes (syndactyly),
- Presence of ovarian and/or cardiac fibroids,
- Eye anomalies
- lymphomesenteric or pleural cysts
How is basal cell nevus syndrome treated?
Since sufferers of basal cell nevus syndrome suffer from the constant formation of basal cell carcinomas, frequent operations are necessary, at which sometimes large areas of skin also have to be transplanted. As a further treatment option, electrochemotherapy can be used for . Especially for the treatment of medullary blastomas, surgery is performed in combination with chemotherapy, while for cysts of the jaw and fibromas of the ovaries, surgical removal is sufficient. If there is a fibroma of the heart, regular cardiological check-ups are sufficient.
The following treatment methods can also be used:
- Cryotherapy: Cold therapy in which the use of cold stimuli is intended to produce a therapeutic effect.
- Photodynamic therapy: Here, a photosensitiser is applied to the skin and irradiated with a special light. In reaction with the oxygen present in the skin, tissue-damaging (cytotoxic) substances are produced which are supposed to attack the tumour tissue.
- medicinal treatment: for example, with topically applied Imiquimod or 5-fluorouracil. The application of imiquimod is supposed to activate the inflammatory cells of the skin, thereby enabling the cells to destroy superficially growing basaliomas. However, this form of treatment is only effective on superficially growing basal cell carcinomas, whereas basal cell carcinomas that have grown deep into the skin can no longer be treated.
Cold,
laser, but also photodynamic therapies can support the surgical
removal of a basal cell carcinoma. Radiotherapies
are avoided if possible because they increase the risk of developing
basal cell carcinoma in the irradiated area.
What are the complications of basal cell nevus syndrome?
Basal cell nevus syndrome can lead to the development of medulloblastomas as early as in childhood . On average, this affects between 5 and 10 percent of all patients.
What should patients with basal cell nevus syndrome pay special attention to?
People with basal cell nevus syndrome, should avoid direct sunlight . This can reduce the risk of developing basal cell nevus syndrome. In this way, the risk of basal cell carcinoma developing can be reduced.
