What is a beta cell tumour?
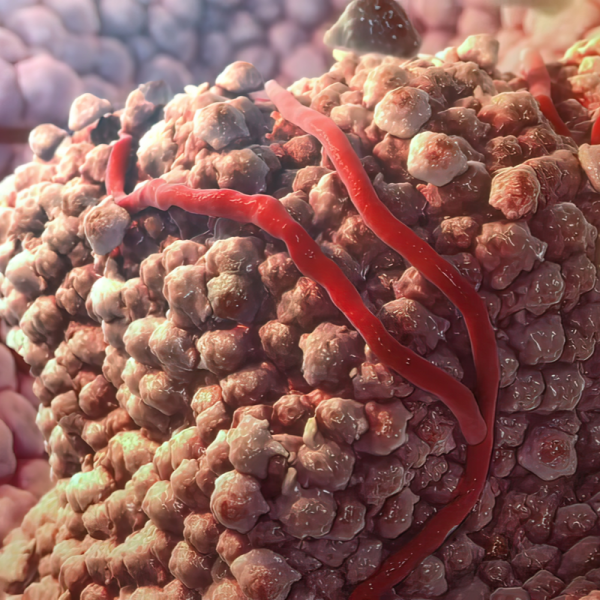
Beta cells are located in the so-called Lagerhans islets of the pancreas and are responsible for the production of the hormone insulin. Insulin lowers blood sugar levels, which means that beta cells play a central role in regulating blood sugar levels. A beta-cell tumour therefore forms in the pancreas and is also called an insulinoma. The beta-cell tumour occurs in 1 to 4 cases per 1 million inhabitants and is therefore rather a rare tumour. People in the 5th and 6th decade of life in particular have an increased risk of developing a beta-cell tumour, with about 10 percent of all insulinomas being malignant. Usually, a beta-cell tumour should be surgically removed, but it can also be inhibited in its growth by drugs called insulin secretions.
What are beta cells responsible for?
Beta cells are the insulin-producing cells of the pancreas. They are responsible for the production of insulin. If the function of the beta cells is disturbed, various forms of diabetes mellitus can develop. In this case, insulin deficiency leads to greatly increased blood sugar levels. Doctors distinguish between the following two types of diabetes:
- Type 1 diabetes: results from an absolute insulin deficiency of the beta cells in the pancreas (Lagerhans islets). Blood sugar rises when about 80 percent of all beta cells are destroyed. Type 1 diabetes can have hereditary causes.
- Type 2 diabetes: is one of the most common forms of diabetes, which usually only sets in at an older age. Type 2 diabetes develops due to an imbalance in insulin secretion and a worsening insulin effect (insulin resistance). Risk factors for the development of type 2 diabetes are obesity, high blood pressure and a dyslipidemia.Type 2 dibates can trigger premature hardening of the arteries (arteriosclerosis) and increase the risk of heart attack and stroke.
What symptoms does a beta-cell tumour cause?
A typical sign of a beta-cell tumour is spontaneous hypoglycaemia, which occurs more frequently during fasting. This is a hypoglycaemia which, in particularly severe cases, can even lead to impaired consciousness or even coma or fainting (syncope). Other signs of hypoglycaemia are:
- Tremors,
- Sweating,
- Increase in blood pressure,
- Heart palpitations (tachycardia),
- inner restlessness,
- Anxiety,
- Hyperventilation,
- a feeling of warmth.
Furthermore, dizziness, headaches, confusion as well as thought and speech disorders and/or a lack of concentration can also indicate hypoglycaemia. In addition to hypoglycaemia, hunger, nausea and vomiting as well as visual disturbances and drowsiness can also be symptoms of a beta-cell tumour.
How is a beta-cell tumour diagnosed?
If there are signs of low blood sugar (hypoglycaemia), the causes must be clarified by a doctor. As a rule, a so-called starvation test is carried out for this purpose, in which the blood glucose as well as the insulin and pro-insulin levels in the blood are examined at regular intervals. Since the majority of those affected do not have any symptoms, i.e. signs of hypoglycaemia, the patient usually has to be hospitalised for 48 to 72 hours to carry out this fasting test in order to make the diagnosis. A beta-cell tumour can be diagnosed by demonstrating marked insulin secretion in the presence of hypoglycaemia. Usually, should the majority of patients have a beta-cell tumour, symptoms of hypoglycaemia will develop within the first 24 hours.
How is a beta-cell tumour treated?
The first choice of treatment is the complete, or extensive, removal of the tumour. This includes the removal of all affected lymph nodes and any liver metastases. Extensive surgery and removal of the tumour promises a cure rate of up to 90 percent. However, the prerequisite for this is that the tumour is precisely localised. Imaging procedures such as computer tomography (CT) or magnetic resonance imaging (MRI) can be used for this purpose. In 60 to 70 percent of all cases, the location of the tumour can be indicated by means of a CT or an MRI. However, it is also possible to localise a beta-cell tumour by means of a so-called endosonography. This is a special type of ultrasound examination that is performed from the inside.
If surgery is not possible, medication can also be administered, such as taking somatostatin analogues to inhibit the hormones and/or diazoxide. Taking diazoxide may also be prescribed if hypoglycaemia persists despite successful surgery. Chemotherapy and dietary measures may also be prescribed. Dietary measures include, above all, the frequent distribution of smaller meals throughout the day.
As a newer treatment method, some clinics also offer therapy with dendritic cells. The so-called dendritic cell therapy is an immunological treatment method in which the dendritic cells are supposed to recognise the degenerated tumour cells in the body and trigger an immune reaction against these cells in order to destroy them. To do this, the dendritic cells are obtained from the body's own blood by isolating the monocytes in the blood. These monocytes are then grown into dendritic cells in the laboratory and injected into the patient.
What is the prognosis for a beta-cell tumour?
Since a beta-cell tumour is not only benign in most cases, but also smaller than two centimetres in more than 90 percent of all cases, the prognosis is good. If the tumour has been completely removed by surgery, the patients are considered cured.
