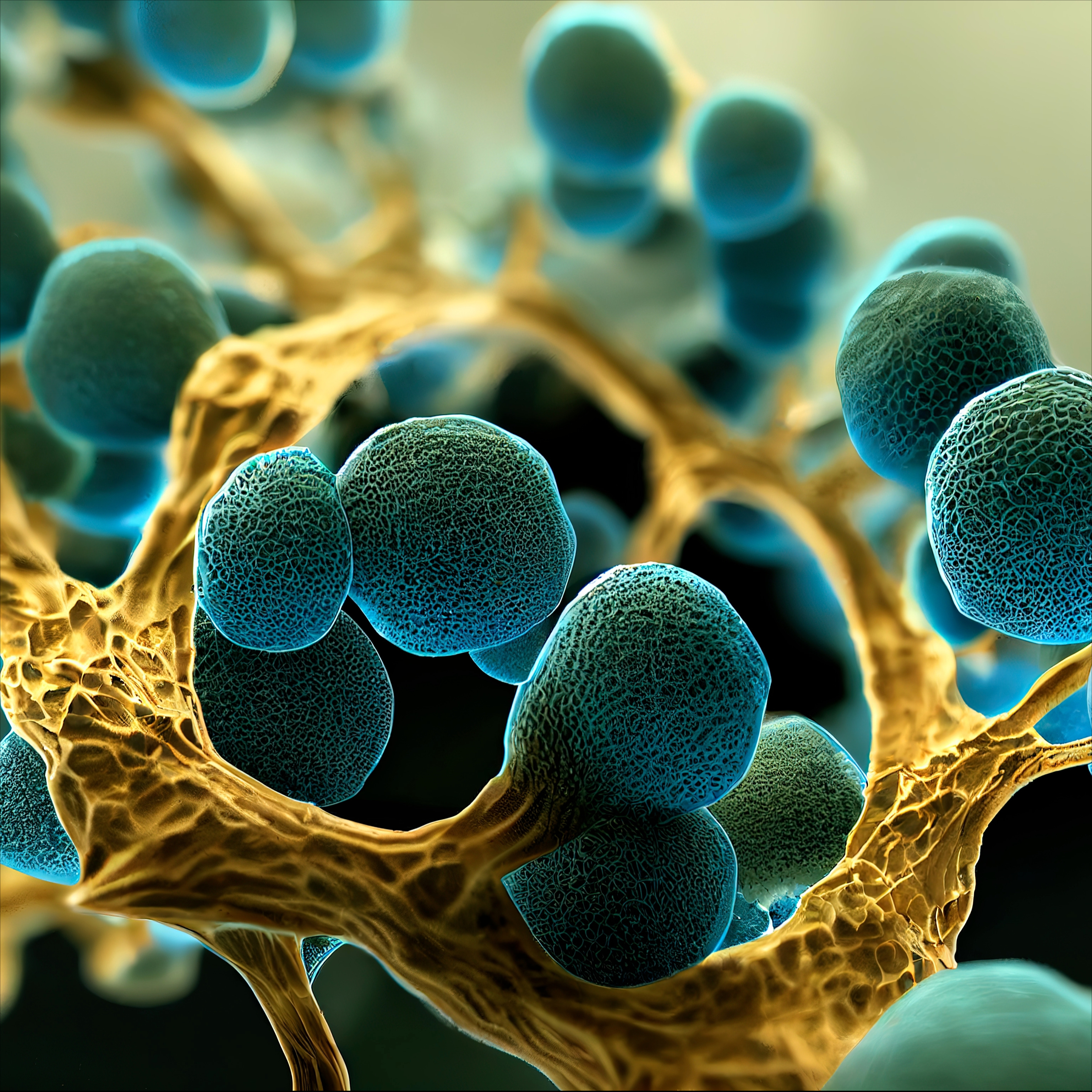
Introduction: What is Candida Albicans?
Candida Albicans is a yeast fungus that occurs naturally in the human body. These
microorganisms are normally harmless and live in symbiosis with our
immune system. They are mainly found on mucous membranes such as in the mouth, intestines and in the
vagina. Under certain conditions, however, Candida Albicans can grow excessively and cause
infections.
Most people do not realise how common Candida Albicans actually is.
studies show that around 70% of the population carry this fungus. Normally,
our immune system keeps the growth of Candida in check. But if the balance
is disturbed, it can lead to so-called candidiasis, an infection that can affect various
parts of the body.
Candida Albicans has the ability to adapt to a wide variety of environments,
which makes it particularly resilient. One example of this is its ability to form
biofilms, a kind of protective layer that shields it from the immune system and medication. These
biofilms are often the reason why Candida infections are difficult to treat and
can recur.
Another remarkable feature of Candida Albicans is its ability to switch between a
yeast-like and a filamentous form. This dimorphism allows it to spread
more efficiently throughout the body and infect different tissues.
In the next sections, we will take a closer look at the causes and
risk factors that can lead to a Candida infection, the typical symptoms and how
to diagnose and treat a Candida infection.
Causes and risk factors for Candida infections
Candida infections can be favoured by a variety of causes and risk factors
. One of the most important factors is a weakened immune system. People with
diseases such as HIV/AIDS, diabetes or cancer are particularly susceptible, as their bodies are less
able to control the growth of Candida Albicans.
Certain medications can also increase the risk. These include antibiotics, which not
only kill harmful bacteria, but also beneficial microorganisms in the body. This can
disrupt the natural balance of the microflora and give Candida albicans the opportunity to
multiply. Corticosteroids and immunosuppressants have a similar effect, weakening the
immune system and thus opening the door to infections.
Hormonal changes also play a major role. Pregnancy, menstruation
and the use of hormonal contraceptives can change the balance of
microorganisms in the vagina and increase the risk of a Candida infection. Stress
and unhealthy eating habits, especially a diet high in sugar, can also
promote the growth of Candida Albicans.
Another risk factor is the wearing of tight or synthetic clothing, which impedes the ventilation
of the skin and creates a moist environment that favours the growth of Candida.
Hygiene habits such as excessive showering or the use of perfumed
hygiene products can disrupt the natural protective barrier of the skin and mucous membranes and
thus increase the risk of infection.
Finally, age also plays a role. Babies and older people often have a less
robust immune system, which makes them more susceptible to Candida infections. For example, babies can
develop thrush, a Candida infection in the mouth, while older adults
are more susceptible to fungal skin and nail infections.
By recognising and avoiding these risk factors, you can significantly reduce the risk of a Candida
infection.
Symptoms and diagnosis of Candida Albicans
Candida infections can cause different symptoms
depending on the area of the body affected. The most common symptoms include itching, redness and swelling of the
affected areas of skin or mucous membranes. In the case of vaginal infections, increased,
whitish discharge and burning are typical signs. In the oral cavity, known as oral thrush,
white, wipeable coatings may appear on the tongue and oral mucosa, accompanied
by pain and difficulty swallowing.
Skin infections caused by Candida Albicans often manifest as red, itchy rashes that
develop in moist skin folds such as under the breasts, in the groin area or between the
toes. In systemic infections affecting internal organs, symptoms
such as fever, chills and general weakness may occur. This form is particularly
dangerous and often occurs in severely immunocompromised individuals.
A Candida infection is usually diagnosed by clinical examination and
analysing samples from the affected area. A microscopic smear can visualise
Candida cells, while a culture on special nutrient media enables growth
and identification of the pathogen. If a systemic infection is suspected,
blood cultures and imaging procedures such as ultrasound or CT scans are necessary to confirm the
diagnosis and determine the extent of the infection.
Early and accurate diagnosis is crucial to initiate the right treatment
and avoid complications. A multidisciplinary approach involving dermatologists, gynaecologists
and infectious disease specialists can help to find the optimal therapy for the individual
patient.
Treatment options and prevention of Candida Albicans
The treatment of Candida infections varies depending on the severity and the affected
body region. Superficial infections such as skin or vaginal fungus are often treated with
antifungals. These medications are available in various forms, including
creams, ointments, tablets and suppositories. Common active ingredients include clotrimazole,
fluconazole and nystatin. A typical course of treatment is usually one to two
weeks, but can vary depending on the severity of the infection.
For systemic Candida infections, which can be life-threatening, stronger
antifungal drugs such as amphotericin B or echinocandins are required. These drugs are
usually administered intravenously and require close monitoring by medical
professionals. Treatment can take several weeks to months, depending on the
spread and the patient's general state of health.
Prevention plays a crucial role in dealing with Candida Albicans. A healthy
lifestyle strengthens the immune system and reduces the risk of infection. This includes a
balanced diet, regular exercise and sufficient sleep. Avoiding
excessive sugar and alcohol consumption can also be helpful, as Candida Albicans
uses sugar as its main food source.
Hygiene measures are also important. Wearing loose, breathable clothing
and avoiding synthetic materials can inhibit the growth of Candida.
Intimate hygiene should be carried out carefully, but not excessively, to maintain the natural
balance of microflora. The use of perfumed hygiene products
should be avoided.
Particular care should be taken when taking antibiotics, as these can disrupt the balance of
microorganisms in the body. Accompanying probiotic therapy can help to maintain the
beneficial intestinal flora and minimise the risk of a Candida infection.
Regular medical check-ups and open communication with the doctor are also
essential in order to take measures for prevention and treatment at an early stage.
Natural remedies and diet to combat Candida Albicans
Natural remedies and an adapted diet can play an important role in combating
Candida Albicans. One of the most effective strategies is the so-called Candida diet.
This diet aims to minimise the sugar content in the body, as sugar is the
main food source for Candida Albicans. It is therefore advisable to reduce the consumption of
refined sugar, white flour products and highly processed foods
or avoid them completely.
Instead, the diet should be rich in fibre-rich foods such as vegetables,
wholemeal products and pulses. Garlic is a particularly effective
food as it contains allicin, a substance with strong antifungal properties.
Coconut oil, which contains lauric acid and caprylic acid, can also inhibit the growth of Candida
albicans.
Probiotics are another important element in the fight against Candida. These beneficial
bacteria help to restore the balance of the intestinal flora and strengthen the
immune system. Yoghurt with live cultures, kefir and fermented foods
such as sauerkraut and kimchi are excellent sources of probiotics.
Herbs and food supplements can also provide support. Oregano oil, which contains
carvacrol and thymol, has strong antifungal properties. Also
grapefruit seed extract and Pau D'Arco tea are often recommended as they can effectively inhibit the growth of
Candida Albicans.
In addition to the diet, lifestyle habits should also be adapted. Regular
exercise, adequate sleep and stress management are crucial to strengthen the
immune system and minimise the risk of Candida infection.
By incorporating these natural remedies and dietary adjustments into your daily routine,
you can significantly reduce the risk of Candida overgrowth and help heal
.
Frequently asked questions and myths about Candida Albicans
- Can anyone get Candida Albicans?
Yes, Candida Albicans is a yeast fungus that occurs naturally in most human bodies . However, it does not lead to infection in everyone. A healthy immune system keeps the fungal population in check. In immunocompromised individuals, however, it can more easily lead to infections. - Can a Candida infection be caused by eating sugar?
Sugar promotes the growth of Candida Albicans as it is a major food source for the fungus . A high-sugar diet can increase the risk of infection, but is not the sole trigger. Other factors such as a weakened immune system or taking antibiotics also play a role. - Are Candida infections contagious?
Candida infections are generally not contagious. The fungus is often caused by the excessive proliferation of Candida cells already present in the body. In rare cases an infection can be transmitted through direct contact, for example from the mother to the child during birth. - Do home remedies work against Candida Albicans?
There are numerous home remedies that can help to alleviate Candida infections. Garlic, coconut oil and probiotics are some examples that are recommended due to their antifungal properties. However, you should consult a doctor if you have severe or recurrent infections. - Is a Candida diet necessary?
A Candida diet can help control the growth of the fungus by reducing the sugar content in the body. A balanced diet rich in fibre and probiotic foods can strengthen the immune system and reduce the risk of infection . - Myths about Candida Albicans:
A common myth is that Candida infections only affect women. In fact, men and children can also be affected. Another myth is that all yeast infections are serious. Many infections are mild and can be easily treated if they are recognised early.
These frequently asked questions and debunking of myths should help to improve awareness
and understanding of Candida Albicans and contribute to effective prevention and
treatment.
Source list:
https://flexikon.doccheck.com/de/Candida_albicans, https://www.rki.de/DE/Content/InfAZ/P/
fungal_infections/candida_spp.html
https://www.gesundheit.gv.at/krankheiten/immunsystem/
venereal_diseases/candida-albicans.html
https://www.usz.ch/krankheit/candida-albicans/
https://de.wikipedia.org/wiki/Candida_albicans
https://www.gesundheitsforschung-bmbf.de/de/
when-the-fungal-infection-becomes-a-life-threat-9687.php
https://www.leibniz-hki.de/de/pressemitteilung/
toxin-of-candida-albicans-plays-a-special-role-in-the-colonisation-of-the-digestive-tract.
html
https://holstenpharma.de/wp-content/uploads/2018/05/Holsten-
Pharma-Candida-albicans-Ein-Ratgeber-fuer-Betroffene.pdf
https://www.haut-undallergiehilfe.
en/blog/skin-diseases/157-candida-albicans
Become a member now
As a member, you will receive further information and frequencies on this topic! Log in here!



