What are cervical polyps?
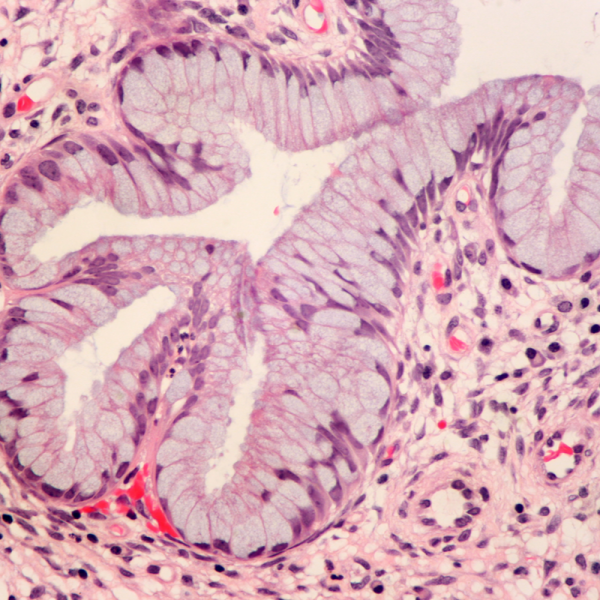
Doctors refer to cervical polyps as finger-like tissue growths that occur in the passageway of the cervix and are usually less than one centimetre in diameter. Cervical polyps occur in 2 to 5 percent of all women due to infection or chronic inflammation and are always benign in most cases. Cervical polyps can cause bleeding or a purulent discharge and are diagnosed during a gynaecological pelvic examination. There is an increased risk of developing cervical polyps, especially after the menopause, between the ages of 45 and 60.
How do cervical polyps develop?
Cervical polyps are caused by the increased growth of mucous membrane cells. Especially in the fertile years of life, polyps can grow due to the high cell division activity of the uterine mucosa, but these usually disappear again on their own during menstruation. The polyps, which are usually less than one centimetre in diameter, are more likely to appear on the cervix, which explains why they are called cervical polyps. They either grow on a stalk, sit on the lining of the uterus or hang down into the vagina.
What symptoms do cervical polyps cause?
In most cases, cervical polyps do not cause any symptoms except bleeding or a purulent discharge. The bleeding can occur after sexual intercourse or between menstrual periods. In rare cases, the cervical polyps can become inflamed and cause a purulent vaginal discharge. This is especially the case with pedunculated polyps that have twisted around themselves, which can trigger cramp-like, colicky pain or cause a feeling of pressure in the lower abdomen. Smaller polyps in particular usually go away on their own with menstrual bleeding.
How are cervical polyps diagnosed?
Cervical polyps are usually diagnosed during a gynaecological pelvic examination. If they are cervical polyps that cause discharge or bleeding, they are removed immediately with forceps. To detect cervical polyps early, women should have regular gynaecological examinations.
How are cervical polyps treated?
Cervical polyps can be removed during a gynaecological pelvic examination using simple forceps, without the need for anaesthetic. If, in rare cases, bleeding occurs, the affected area is treated with a corrosive substance such as silver nitrate.
The removed polyps are then examined in the laboratory to make sure that they do not cause cancer. If the bleeding and discharge do not subside even after the successful removal of the cervical polyps, a sample of the lining of the uterus (endometrium) is taken and a biopsy is performed to rule out the possibility that the symptoms are caused by endometrial cancer.
| Pathogen | Source | Members - Area |
|---|---|---|
| Polyps General 3 | CAFL | As an NLS member you have direct access to these frequency lists |
| Polyps General 2 | CAFL | As an NLS member you have direct access to these frequency lists |
| Polyps General 1 | CAFL | As an NLS member you have direct access to these frequency lists |
| Polyps General | EDTFL | As an NLS member you have direct access to these frequency lists |
| Polyps Growths | XTRA | As an NLS member you have direct access to these frequency lists |
