What is endometrial carcinoma?
Endometrial carcinoma is also colloquially called uterine cancer and refers to the malignant tumour that originates from the inner mucosal layer of the uterus. Uterine cancer is one of the most common malignant cancers of the genital tract in women. The average age at which endometrial cancer is diagnosed is between 65 and 70 years.
What risk factors favour the development of endometrial carcinoma?
There are both endogenous and exogenous risk factors that can favour the development of endometrial carcinoma. Endogenous risk factors include overweight (obesity), diabetes mellitus, early onset of menstrual bleeding and/or late onset of menopause, no pregnancies and the presence of polycystic ovarian syndrome and/or oestrogen-secreting tumours.
Exogenous risk factors include no natural onset menstrual cycle, but oestrogen replacement therapy and/or previous radiotherapy. In summary, therefore, women who have been pregnant have a lower risk of developing endometrial cancer than women who have not experienced pregnancy. The risk of developing cervical cancer decreases significantly with the number of pregnancies. However, long-term use of the female sex hormone oestrogen also increases the risk of developing endometrial cancer.
How can the development of endometrial carcinoma be prevented?
Although there are no targeted screening tests, such as screening for uterine cancer, the disease can still be prevented as follows:
- Reducing body weight, such as through regular physical activity,
- various contraceptive methods, such as the contraceptive pill, which usually consists of a combination of oestrogen and progestogen,
- Birth of a child at a late age
What symptoms suggest endometrial cancer?
Any form of bleeding, whether it occurs in the premenopause or in the postmenopause, can indicate endometrial carcinoma. In 5 per cent of all cases of disease, bleeding in the early postmenopause turns out to be a symptom of endometrial carcinoma, while in the late postmenopause as many as 50 per cent of all cancers manifest themselves through bleeding. One in five endometrial carcinomas, on the other hand, causes no symptoms at all and is usually diagnosed only by chance. If the endometrial cancer is more advanced, increased discharge and pain may indicate cervical cancer. Since endometrial carcinoma usually manifests itself through these symptoms, it is important to have them diagnosed by a doctor at an early stage.
How is endometrial cancer diagnosed?
If there is a suspicion of endometrial carcinoma due to bleeding, for example, gynaecological examinations are first carried out to clarify whether the bleeding is coming from the uterus. For this purpose, the gynaecologist usually performs an ultrasound, which is followed by a hysteroscopy if the findings are abnormal. During this operation, the uterine cavity is usually scraped and, if necessary, the bladder and rectum are examined to see how far advanced the endometrial carcinoma is.
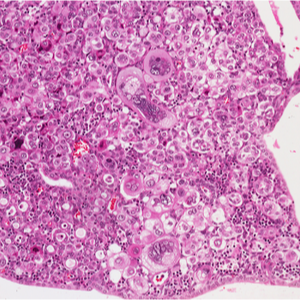
Only after the pathologist has examined the scraped material can a final diagnosis be made, which also defines the degree of differentiation of the endometrial carcinoma. This is usually followed by further diagnostics using additional imaging procedures such as magnetic resonance imaging (MRI) and/or X-rays to determine whether the tumour has already metastasised.
What tumour stages is endometrial carcinoma classified into?
Endometrial carcinoma is usually divided into two types:
- Type I tumours: these occur most often in younger patients, before the onset of menopause. They usually tend to be overweight. Type I tumours are usually low-malignant.
- Type II tumours: they are usually highly malignant (malignant) and occur mainly in older women.
How is endometrial carcinoma treated?
Endometrial carcinoma can be treated either by surgery with follow-up radiotherapy or by primary radiotherapy. Since surgical treatment usually has a better prognosis, it is preferable to radiation treatment. However, there are some patients who cannot be operated on because of their general health or other contraindications.
If it is an early-stage tumour, it is usually treated by partial or complete surgical removal of the uterus (hysterectomy). In addition, the ovaries (adnexa) are also removed during this procedure. In most cases, the operation is performed by laparoscopy from the vagina, which means that an abdominal incision can be avoided. If the tumour is already more advanced, the lymph nodes must also be removed. If the lymph nodes were affected by the tumour, post-operative radiation may also be necessary.
In addition to surgery and chemotherapy, radiotherapy is also one of the treatment options for endometrial carcinoma. Radiation therapy can also be used to reduce the size of the tumour before an operation or to destroy microscopic tumour remnants after the operation. As a palliative method, radiotherapy is intended to alleviate the symptoms if, for example, the tumour can no longer be cured due to its advanced stage. Which treatment method is used depends not only on the stage of the tumour, but also on the patient's general state of health.
What is the prognosis for endometrial cancer?
An endometrial carcinoma that has already metastasised and the patient is already relatively old has a poor prognosis for a complete cure. In general, the average 5-year survival rate after treatment of stage I or II endometrial carcinoma is between 70 and 95 per cent. Stage III or IV endometrial cancer, on the other hand, has an average 5-year survival rate between 10 and 60 per cent. As a rule, about 63 percent of all patients remain tumour-free for at least 5 years after therapy.
