Basic knowledge about skin fungus
Symptoms, causes and prevention
Introduction to skin fungus:
Understanding the basics
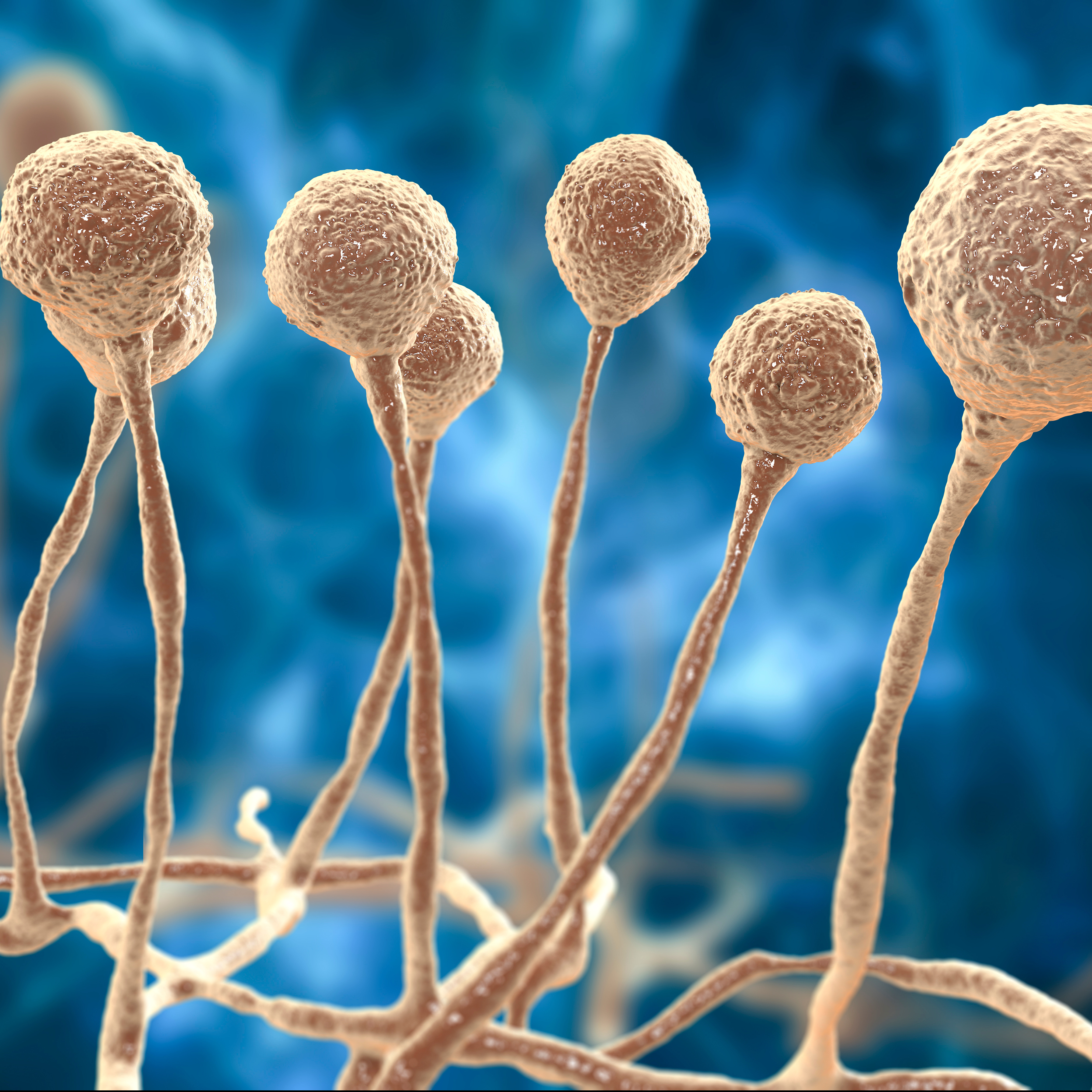
Skin fungus, also known as dermatophytosis or tinea, is a common skin infection caused by various types of fungi.
These fungi can affect the skin, hair and nails and lead to unpleasant symptoms such as itching, redness and scaly skin lesions.
Mycosis occurs worldwide and can affect people of all ages, although certain groups are at higher risk.
what is dermatomycosis?
Athlete's foot is caused by dermatophytes, a specialised group of fungi that are able to break down keratin, a protein in the skin.
These fungi thrive in warm, moist environments and can be transmitted through direct skin contact or through contact with contaminated objects such as towels, clothing or floors.
Why is skin fungus a problem?
Skin fungus is not just a cosmetic problem, but can lead to serious complications if left untreated.
Particularly in people with a weakened immune system, such as older people or patients with chronic illnesses, a fungal skin infection can cause serious health problems.
According to a study by the Robert Koch Institute (RKI), fungal skin infections are one of the most common skin diseases in Germany and affect millions of people every year.
Common symptoms and signs
Typical symptoms of a fungal skin infection are:
- Itching and burning
- Redness and inflammation
- Scaly or cracked skin
- Ring-shaped skin rashes (with tinea corporis)
- Thickened and discoloured nails (with nail fungus)
Recognising these symptoms is the first step in the effective treatment and prevention of fungal skin infections.
In the upcoming sections of this blog post, we will detail the different types of fungal skin infections, their causes and risk factors, as well as the best methods for diagnosis, treatment and prevention.
Common types of skin fungus and their symptoms
Skin fungus can occur in various forms, each with its own characteristic symptoms. Here are the most common types of skin fungus and their symptoms:
Tinea corporis (ringworm)
Tinea corporis, also known as ringworm, is one of the most well-known forms of skin fungus. It manifests as a ring-shaped rash with a clear, scaly border and an often lighter-coloured centre. Symptoms include:
- Itching and burning: Particularly intense around the edge of the rash.
- Circular redness: The affected areas of skin are reddish and scaly.
- Scaling: The skin in the affected area may become dry and scaly.
Tinea pedis (athlete's foot)
Tinea pedis, also known as athlete's foot, mainly affects the feet, especially the skin between the toes.
This type of skin fungus is particularly common among athletes, hence the name "athlete's foot".
Symptoms are:
- Itching and burning: Especially between the toes.
- Cracked skin: The skin can become cracked and sore.
- Blistering: In severe cases, small blisters may form.
Tinea cruris (jock itch)
Tinea cruris, often referred to as jock itch, affects the groin area and inner thighs. This infection is more common in men and is favoured by tight-fitting clothing and heavy sweating.
Signs include:
- Redness and swelling: especially in the groin area.
- Itching: Intense itching may occur.
- Scaly skin: The affected areas of skin may be scaly and dry.
Tinea capitis (scalp fungus)
Tinea capitis affects the scalp and is particularly common in children.
Symptoms are:
- Round, bald patches: These can be scaly and reddened.
- Itching: The scalp can itch intensely.
- Inflammation: In severe cases, inflamed, purulent bumps may form.
Onychomycosis (nail fungus)
Onychomycosis affects the nails and can affect both fingernails and toenails.
This infection leads to thickened, discoloured and brittle nails.
The main symptoms are
- Thickened nails: the nails become thicker and uneven.
- Discolouration: Nails may become yellowish, greenish or brownish in colour.
- Crumbling nails: The affected nails may break or split easily.
These different types of skin fungus require specific treatment approaches, which we will explain in more detail in the following sections.
Causes and risk factors associated with skin fungus
Skin fungus, medically known as dermatophytosis, is favoured by various factors.
These factors can be divided into two main categories: external causes and individual risk factors.
Understanding these causes and risk factors is crucial to preventing and effectively treating infection.
External causes
- Moisture and heat: Skin fungi thrive particularly well in warm and humid environments. Wearing tight-fitting clothing, sweating profusely and spending time in humid areas such as swimming pools or saunas can encourage the growth of fungi.
- Direct contact: Cutaneous fungus can be transmitted through direct skin contact with an infected person or animal. Contact with contaminated objects such as towels, clothing or floors can also lead to infection.
- Poor hygiene: Inadequate hygiene, such as changing clothes infrequently or not drying the skin after showering, can increase the risk of a fungal skin infection.
Individual risk factors
- Weakened immune system: People with a weakened immune system, such as older people, diabetes patients or people taking immunosuppressive medication, are more susceptible to fungal skin infections.
- Skin injuries: Small cuts, scrapes or other skin injuries provide fungi with a portal of entry, increasing the risk of infection.
- Chronic diseases: People with chronic conditions such as diabetes or circulatory disorders are at a higher risk of fungal skin infections as their skin is often more susceptible.
- Genetic predisposition: Some people are genetically more susceptible to fungal skin infections. Studies have shown that familial clusters of fungal skin infections exist.
Risk factors at a glance
- Moisture and heat: Frequent wearing of tight clothing, heavy sweating
- Direct contact: Contact with infected people or animals, contaminated objects
- Weakened immune system: Elderly people, diabetes patients, people on immunosuppressive medication
- Skin injuries: Small cuts, scratches, skin tears
- Chronic diseases: Diabetes, circulatory disorders
- Genetic predisposition: Familial clustering of fungal skin infections
Knowledge of these causes and risk factors is crucial in order to take preventative measures and effectively combat fungal skin infections.
In the next section, we will take a closer look at the various diagnostic methods for identifying skin fungus.
Diagnostic methods for identifying skin fungus
The diagnosis of skin fungus, also known as dermatophytosis, requires a thorough examination by a dermatologist. There are various methods to accurately identify fungal skin infections:
Clinical examination
An experienced dermatologist can often diagnose dermatophytosis by visual inspection. Typical signs such as ring-shaped rashes, scaly skin or thickened nails provide the first clues. This method is quick and non-invasive, but only provides a preliminary diagnosis.
Microscopic examination
for a more precise diagnosis, a doctor can take skin samples and examine them under a microscope. This involves dissolving small flakes of skin, hair samples or pieces of nail in a potassium hydroxide (KOH) solution to visualise the fungal structures.
This method is reliable and can be carried out within a few minutes.
### Culture examination
A culture examination is another precise method for identifying skin fungi. The skin samples taken are incubated on a culture medium to promote the growth of the fungi.
This method can take up to two weeks, but provides accurate results on the specific fungal species.
Wood-light examination
Another diagnostic tool is the wood-light examination. This uses ultraviolet light to illuminate infected areas of skin.
Certain types of fungi fluoresce under this light, making diagnosis easier. This method is particularly useful for scalp infections.
Biopsy
In rare cases, when other methods do not provide clear results, a skin biopsy can be performed. A small piece of skin tissue is removed and examined histologically.
This method is more invasive, but provides comprehensive information about the infection.
With these diagnostic methods, a fungal skin infection can be effectively identified and the appropriate treatment initiated.
Treatment options and home remedies for skin fungus
The treatment of skin fungus, also known as dermatophytosis, requires a combination of medical therapies and home remedies.
Early and targeted treatment is crucial in order to combat the infection quickly and effectively.
Medical treatment options
Antifungal creams and ointments
Topical antifungal agents are the first choice for treating fungal skin infections. These creams and ointments contain active ingredients such as clotrimazole, miconazole or terbinafine, which are applied directly to the affected areas of skin. They work by destroying the cell membranes of the fungi and thus preventing their growth.
Oral antimycotics
In severe or widespread cases, the doctor may prescribe oral antifungals. Drugs such as fluconazole or itraconazole have a systemic effect and are particularly effective for nail fungus or deep skin infections.
These medications should be taken strictly as directed by a doctor to avoid side effects.
Antifungal shampoos
Special antifungal shampoos are helpful for scalp fungus (tinea capitis). These contain active ingredients such as ketoconazole or selenium sulphide and are used regularly to combat the fungi and prevent the infection from flaring up again.
home remedies
in addition to medical treatments, various home remedies can also help to alleviate symptoms and support healing:
Tea tree oil
Tea tree oil has natural antifungal properties. Applying a diluted tea tree oil solution to the affected areas of skin can help fight the fungi and relieve itching.
Garlic
Garlic also has antifungal properties. Applying crushed garlic or garlic extract to the affected areas can aid healing.
Vinegar
A vinegar bath or applying diluted apple cider vinegar to the infected areas can disinfect the skin and inhibit the growth of fungi.
Practical tips for treatment
- maintain hygiene: Regular washing and drying of the skin is crucial.
- Change clothes: Wear fresh, breathable clothing every day to avoid dampness.
- Keep nails short: If you have nail fungus, keep your nails short and clean to prevent it from spreading.
A combination of medical treatment and proven home remedies can effectively treat skin fungus.
It is important to carry out the treatment consistently and maintain hygiene to prevent re-infection.
Preventive measures and tips for avoiding skin fungus
By taking simple but effective preventative measures, you can significantly reduce the risk of infection.
Here are some proven strategies and tips for preventing skin fungus:
Hygiene measures
- Regular washing and drying: Make sure you wash your skin thoroughly and dry it completely every day, especially after swimming or exercising. Moisture is a breeding ground for fungi.
- Clean clothes: Change your clothes and underwear daily. Wear breathable fabrics such as cotton to avoid sweat build-up.
- Do not share towels and clothing: Avoid sharing towels, bed linen or clothing with others to prevent transmission.
Source list:
- https://www.netdoktor.de/krankheiten/hautpilz/
- https://www.canesten.de/hautpilz
- https://www.adler-apotheke-kirchheim.de/gesundheitsbibliothek/index/hautpilz/
- https://www.shop-apotheke.com/ratgeber/hautpilz/
- https://www.multilind.de/hauterkrankungen/hautpilz
- https://www.gesundheit.gv.at/krankheiten/haut-haare-naegel/hautpilz.html
- https://www.getmayd.com/krankheiten-symptome/hautpilz/
- https://de.wikipedia.org/wiki/Dermatomykose https://www.multilind.de/hauterkrankungen/hautpilz/ursachen
