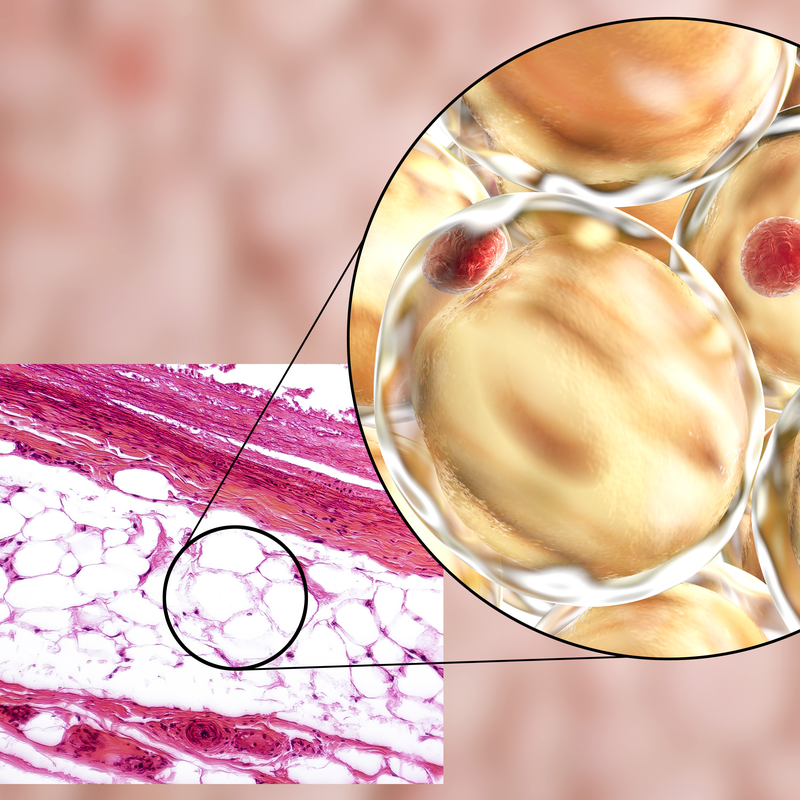
What is a hibernoma?
A hibernoma describes a congenital, rare benign tumour of the fatty tissue (lipoma) that grows very slowly. It forms in adults from scattered remnants of the fetal brown lipoma tissue of the subcutis. A hibernoma usually develops in the subcutaneous tissue or in the musculature, preferably in the trachea or in the mediastinum along the oesophagus and can be between 5 and 10 cm in size. In rare cases, a hibernoma can grow up to 20 cm and also form in the neck or between the shoulder blades. In this case, it usually causes pain due to its pressure. Men are more likely to get hibernomas than women. Hibernomas form more often than average in the 3rd or 4th decade of life. Hibernomas hardly ever occur in children.
What forms can a hibernoma take?
A hibernoma develops from cells with a large cytoplasmic space that is rich in glycogen (carbohydrate stored in the cell ) and phospholipid. The following four tumour forms are distinguished :
- typical hibernoma: characterised by its different degrees of differentiation. The typical hibernoma appears as a uniform, round or oval cell with prominent edges, which is interspersed with coarsely multivacuolated fat cells and represents the most frequent variant of hibernomas, accounting for 82 percent of all cases of the disease.
- myxoid hibernoma: this is a loose, basophilic matrix that has foamy histiocytes (cells of connective tissue) and thick fibrous septa. The myxoid hibernoma occurs mainly in men in the head and neck region.
- spindle cell hibernoma: is a mixed form of a spindle cell lipoma and a hibernoma, which only forms in 2 per cent of all cases and is therefore by far the rarest variant of hibernomas.
- lipoma-like hibernoma: consists of isolated hibernoma cells and most often appears on the thigh.
What causes a hibernoma to form?
A hibernoma develops from brown fatty tissue. The function of brown adipose tissue is to burn fat without shivering, the so-called thermogenesis. Thermogenesis involves the fatty acid-dependent uncoupling of adenosine triphosphate (ATP). This is achieved via the uncoupling protein UCP1 in the mitochondria. As a rule, infants have brown fat deposits, which is why it is assumed that these usually disappear on their own in adulthood. However, in some adults, the presence of brown fat can be detected . If this brown fat grows continuously, hibernomas can develop from it.
Meanwhile, doctors have been able to determine that the development of a hibernoma in some cases is accompanied by chromosomal rearrangements in the long arm of chromosome 11. In addition, the loss of AIP and MEN1 genes is also regarded as an essential cause of the development of a hibernoma.
What are the symptoms of a hibernoma?
A hibernoma is usually asymptomatic. In some cases a hibernoma can cause pain and/or failures of the nerves and blood vessels due to the locally acting compression of the surrounding tissue. This is usually the case when hibernomas gain clinical significance due to their growth in size and begin to exert pressure on neighbouring tissue. Also, hibernomas can manifest themselves through chronic inflammation in the form of lymphocytes.
Where do hibernomas preferentially form?
The slowly progressing, growing, painless mass of a hibernoma forms mainly on the thigh, shoulder, back, chest and neck, as well as on the arms and the region behind the peritoneum (retroperitoneum). In addition, a hibernoma can also appear on the larynx, on the pleura, in the pelvic region as well as on the vulva or the scrotum. Almost 10 percent of all hibernomas are intramuscular.
How is a hibernoma diagnosed?
Since hibernomas are usually asymptomatic, they are often diagnosed as incidental findings only after years of their development. This can happen, for example, through the usual imaging procedures such as an X-ray examination. In a magnetic resonance imaging (MRT) with contrast medium, the hibernoma manifests itself through characteristic features, such as a well-defined, thin capsule, which is permeated by food vessels. If the hibernoma is diagnosed by positron emission tomography (PET), it manifests as a large, well-defined lesion. However, it requires a histological examination, for example by taking a tissue sample (biopsy) and examining it in the laboratory, to make a definite diagnosis. In this biopsy, the hibernoma appears as an encapsulated, rubbery mass that turns yellow to reddish brown when cut.
It is important for a reliable diagnosis that the hibernoma is clearly distinguished from other benign tumour forms . These include lipoma, but also other forms of tumour. These include lipoma, but also haemangioma and angiolipoma.
How is a hibernoma treated?
For the treatment of a hibernoma, surgical removal of the tumour is usually attempted. However, this is only necessary if the patient feels pain. If the hibernoma is asymptomatic , treatment is rarely necessary because the tumour almost never degenerates . If the tumour could be completely removed during an operation , there are usually no recurrences.
What complications can occur with a hibernoma?
A fast-growing hibernoma that also tends to infiltrate neighbouring structures can lead to complications. Also, these types of hibernomas can put pressure on the nerves, resulting in a neuropathic pain.
What are the prognoses for a hibernoma?
If the tumour has not been completely removed surgically, there is a risk of local recurrence. Since no case of metastatic hibernoma has been described in the literature so far, the prognosis is quite favourable.
