What is an insulinoma?
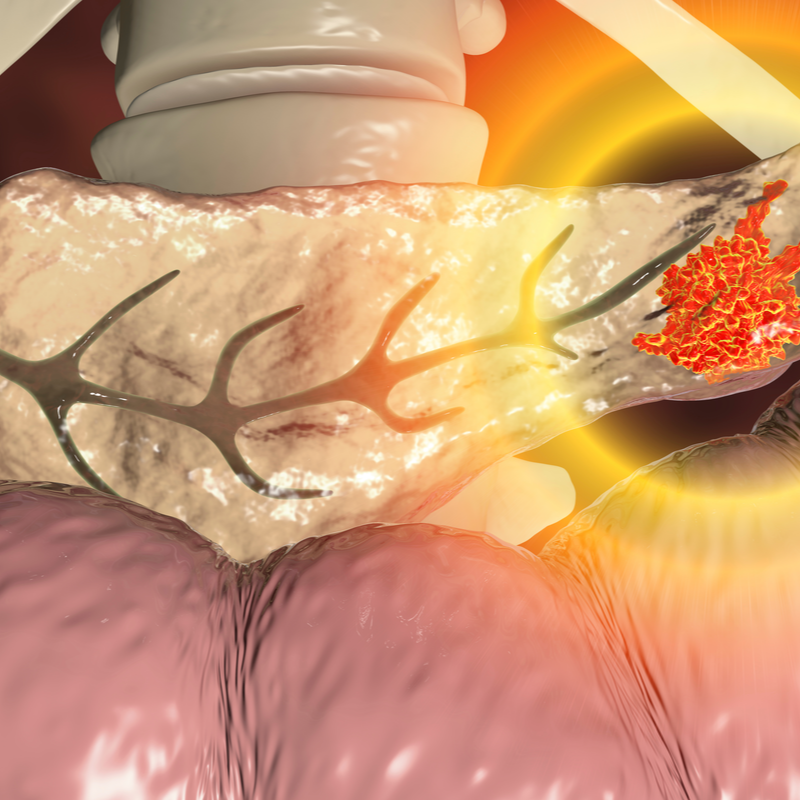
An insulinoma is a beta-cell tumour of the pancreas. Although the tumour is rare, is the most common endocrine pancreatic tumour and secretes insulin in excessive form. Due to the uncontrolled production of insulin, the blood sugar level drops and the patient suffers hypoglycaemia.
An insulinoma forms from islet cells and can be malignant in 10 percent of all cases. In about 90 percent of all cases of disease, the tumour is benign and occurs singly. Otherwise, it is called a multiple microadenoma. An above-average number of insulinomas develop between the ages of 50 , with women developing the disease about twice as often as men.
How does an insulinoma develop?
An insulinoma usually develops from adenomatous degenerated B cells of the islets of Langerhan in the pancreas. As a result of the degeneration, an excess of insulin is produced, which is released from the pancreas directly into the bloodstream. In just under half of all cases of disease, the adenoma produces gastrointestinal hormones, i.e. hormones of the digestive tract, in addition to insulin. These include, for example, the hormones of the vasoactive intestinal peptide (VIP). This is responsible for the muscle relaxation of the stomach, the intestine, the trachea and the bronchi.
Exactly why an insulinoma develops has not yet been clarified. However, it has been proven that insulinomas occur more frequently in the context of multiple endocrine neoplasia (MEN).
Is an insulinoma dangerous?
In 85 percent of all cases of disease, insulinomas are benign and occur solitarily. Only in 6 to 13 percent of all cases does a multiple formation of insulinomas occur. If an insulinoma metastasises, they usually spread into the peripancreatic fatty tissue and into the surrounding organs such as the duodenum or the spleen. Whereby the first metastases can usually be found in the lymph nodes and in the liver.
What does increased insulin production lead to?
A insulinoma produces insulin inside the pancreas. This is a hormone that in healthy people is released into the blood and influences the blood sugar level. This is because the insulin in the bloodstream sends signals to the body to encourage the cells to absorb and process sugar. This process lowers the blood sugar level. In an insulinoma, there is therefore an excess of insulin, i.e. the body cells have more sugar available than they actually need. This unused sugar is usually stored in the form of body fat, which is why many insulinoma patients suffer from overweight (obesity).
What are the symptoms of insulinoma?
An insulinoma typically manifests itself through a form of hypoglycaemia, a so-called fasting hypoglycaemia, which mainly occurs during fasting. This can lead to various symptoms which can be of a psychiatric as well as neurological nature :
- Central nervous system disorders,
- Headaches,
- Visual disturbances,
- Confusion,
- motor weakness and even paralysis,
- Damage to nerve cells in the cerebellum and spinal cord (ataxia),
- marked personality changes up to loss of consciousness, seizures and coma,
- sympathetic stimulation, which manifests itself as weakness, palpitations, sweating, faintness, shakiness, palpitations, hunger as well as nervousness.
Symptoms of an insulinoma can also occur
during the treatment of diabetes mellitus with blood sugar-lowering
drugs.
How is an insulinoma diagnosed?
An insulinoma can be detected by determining the glucose and insulin levels . The test is done as part of a 48- or 72-hour fasting test. This test is usually done as part of an inpatient admission for a maximum of 72 hours. Symptoms develop in 98 percent of all patients suffering from an insulinoma, in 70 to 80 percent of all patients these symptoms already appear within the first 24 hours. The fact that these are symptoms of hypoglycaemia can be determined by the following three factors:
- The complaints manifest themselves during fasting.
- The symptoms indicate hypoglycaemia.
- The intake of carbohydrates alleviates the symptoms.
If
the 48- or 72-hour fasting test should confirm the suspicion of an insulinoma
, this is followed by an endosonography. This
can usually localise the tumour. As an alternative to endosonography
, positron emission tomography (PET)
can also be performed.
How is an insulinoma treated?
If possible, an insulinoma should be surgically removed (resection). As a rule, 90 percent of all patients can be cured by resection. If it is a small, solitary insulinoma, which is close to the surface of the pancreas, it can be enucleated . If it is a large insulinoma, the insulinoma is located deep in the body of the pancreas or the tumour cannot be found , a surgical removal of the pancreas (subtotal pancreatectomy) is performed.
If the hypoglycaemia persists despite the operation, medication can be prescribed to reduce insulin secretion. These include beta blockers, diazoxide, phenytoin, octreotide or calcium channel blockers. Chemotherapy can also be used, although success rates tend to be low.
What is the prognosis for insulinoma?
Unlike pancreatic cancer, an insulinoma has a fairly good prognosis. Since in more than 90 percent of all cases the insulinoma is benign and smaller than two centimetres, the life expectancy is quite good. As a rule, patients are considered cured after the successful surgical removal of the insulinoma. If hypoglycaemia remains undetected and untreated, it can lead to lasting damage to the central nervous system.
