What is islet cell carcinoma?
Islet cell carcinoma is a malignant tumour originating from the pancreas. . Islet cell carcinoma is a rare form of pancreatic cancer that is easily treatable if diagnosed early, and starts in the cells of the pancreas. Islet cell carcinoma can cause the pancreas to produce too much insulin or other hormones .
Islet cell carcinomas that produce hormones are also called functioning tumours. However, if the islet cell carcinomas do not produce hormones, they are called non-functioning tumours. Most of the functioning tumours, i.e. those that produce insulin , are benign. On the other hand, about 90 % of the non-functioning tumours are malignant. Very many of the islet cell carcinomas are non-functioning and produce symptoms and discomfort due to the growing tumour mass and metastases.
How often does islet cell carcinoma occur?
According to Robert Koch Institute, the frequency of islet cell carcinoma is about 16.6 per 100,000 women and 15.8 per 100,000 men. Accordingly, only slightly more women are affected than men.
What risk factors play a role in the development of islet cell carcinoma?
The following risk factors play a major role in the development of islet cell carcinoma:
- Obesity,
- Smoking,
- Chemical noxae such as 2-naphtylamine, DDT, benzidine,
- chronic cholecystitis / pancreatitis,
- genetic recurrent pancreatitis,
- familial clustering, such as Peutz-Jeghers syndrome.
What are the symptoms of islet cell carcinoma?
In general, there are no specific symptoms in the early stages. However, the following may indicate islet cell carcinoma:
- Weight loss,
- Weight loss, fatigue, loss of appetite,
- Jaundice
- belt-shaped pain in the back and upper abdomen.
The islet cell carcinoma is as difficult to diagnose as all pancreatic cancers at an early stage. This is because a doctor will not palpate a patient for a tumour as part of a routine examination . However, if there is a suspicion of islet cell carcinoma, appropriate examinations are carried out to confirm the suspicion and to be able to make a definite diagnosis .
The following examinations are carried out as part of the diagnosis:
- physical examination,
- Self-history and family history,
- Blood tests,
- Biopsy,
- imaging procedures.
The following imaging procedures are used to make the diagnosis:
- Ultrasound of the abdomen,
- endoscopic ultrasound,
- CT, MRI,
- endoscopic retrograde cholangiopancreatoscopy,
- Laparoscopy.
What stages is islet cell carcinoma classified into?
The islet cell carcinoma or pancreatic cancer is divided into five stages . The diagnosis depends on the location and size of the tumour. It also depends on whether the cancer has already metastasised or not:
- Stage 0: Abnormal cells in the pancreas that may develop into a tumour . This stage is also called the pre-cancer stage .
- Stage I: There is a tumour in the pancreas.
- Stage II: The tumour is in the pancreas and has spread to nearest tissues and neighbouring organs or lymph nodes .
- Stage III: The cancer has already spread to the larger blood vessels. Lymph nodes may already be affected.
- Stage IV: In this stage, metastases have formed in distant areas in the body, liver, spleen, lungs or abdominal cavity.
How is islet cell carcinoma treated?
Depending on the stage and localisation of the islet cell carcinoma or pancreatic cancer, the therapy is decided. The general state of health of the patient is also dependent. The primary goal of therapy is to eliminate the cancer. If this is not possible, the aim is to improve the quality of life. The same applies to the prevention of further damage, caused by the growth of the cancer.
The following options are available for treatment:
- surgical removal : The part of the pancreas affected by cancer is surgically removed . The lymph nodes can also be removed during this operation. During this operation, the lymph nodes, which are nearby, can also be removed.
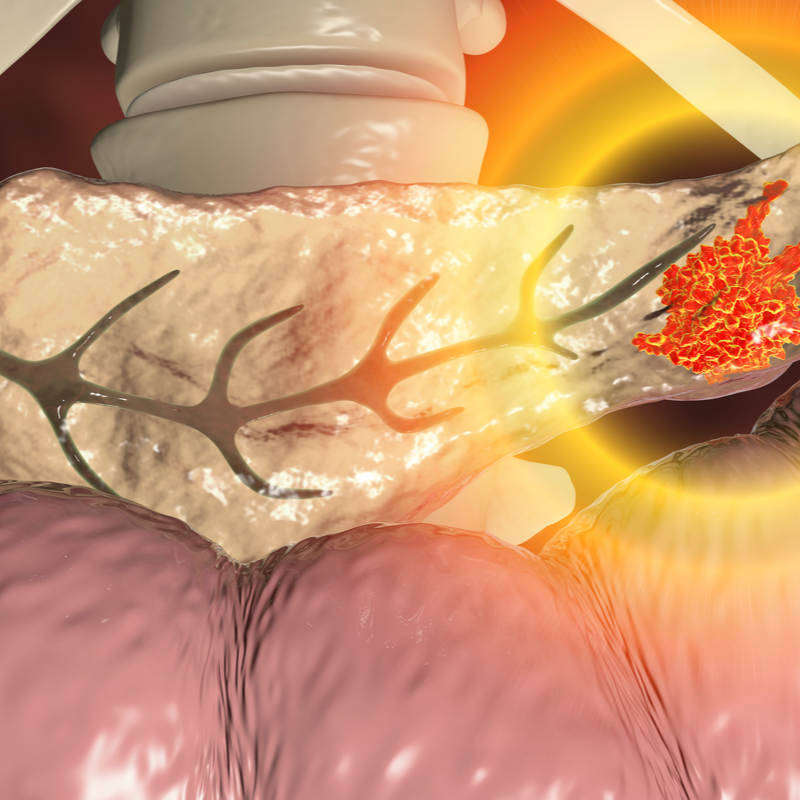
- Radiation therapy: The cancer cells are killed with the help of high-frequency energy.
- targeted therapy: This treatment targets certain proteins or genes that promote cancer growth. On the basis of gene tests carried out , it can be determined whether a targeted treatment is possible.
- palliative therapy: If the cancer has progressed so far that there is no chance of a cure, a treatment is given to alleviate the symptoms. Usually, a combination of the above-mentioned measures is used for this purpose.
How is islet cell carcinoma treated after surgery?
Before especially after surgery, intensive medical monitoring and a careful and slow diet are necessary. A lifelong intake of enteric-coated medication is essential, as there is a pancreatic insufficiency after surgery. In addition, lifelong therapy with insulin will be necessary. The patient's quality of life will remain severely limited overall
What are the complications of islet cell carcinoma?
The islet cell carcinoma causes numerous complications due to its central location in an advanced stage. islet cell carcinoma spreads metastases very early, especially to the peritoneum, liver, but also bones and lungs. Once it has reached a certain size, it will press on the bile duct and the stomach outlet. This leads to nausea and vomiting or even bile flow problems, which lead to jaundice. It is not rare for diabetes mellitus to develop as a further disease due to islet cell carcinoma.
What is the prognosis for islet cell carcinoma?
Since a tumour in the pancreas does not show any symptoms in the early stages, the tumour is often only detected too late. Accordingly, the relative 5-year survival rate is rather unfavourable. In Germany it is about 10 %. Besides mesothelioma, carcinoma of the pancreas has the lowest survival rate of all cancers .
How can islet cell carcinoma be prevented?
The following can be mentioned as preventive measures:
- do not smoke,
- maintain a healthy body weight and avoid being overweight,
- eat a healthy diet.
