What is lymphogranuloma venereum?
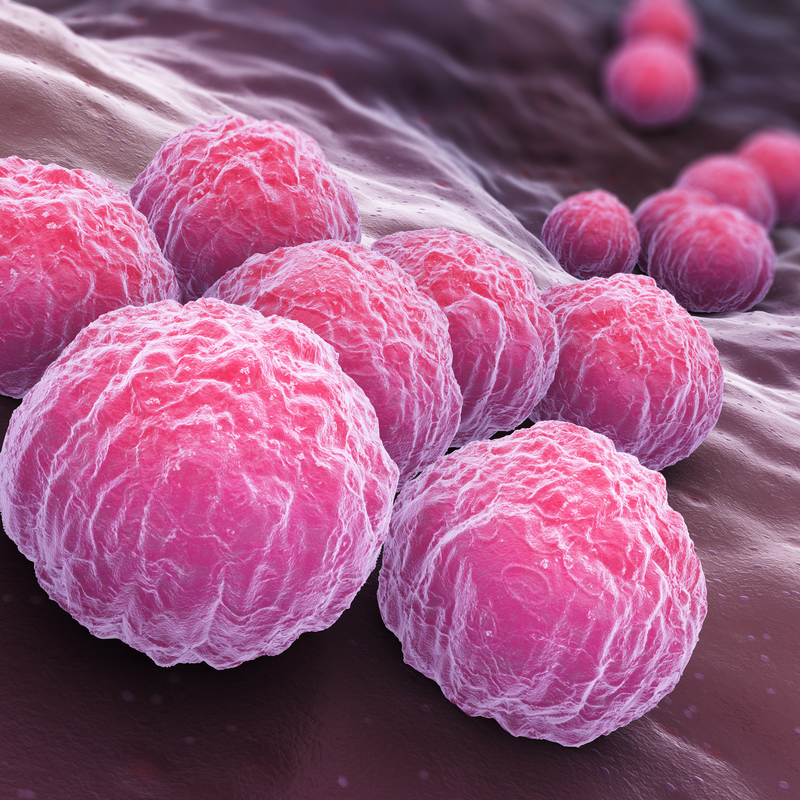
Lymphogranuloma venereum is a classic venereal disease and belongs to a special form of genital chlamydial infection. The disease is particularly widespread in tropical areas, but occurs rather rarely in western countries. A lymphogranuloma venereum is formed by the special subgroups of the pathogen Chlamydia trachomatis . The disease occurs mainly in tropical areas, but is rather rare in western countries. People between the ages of 20 and 30 are infected with the disease with above-average frequency.
How is lymphogranuloma venereum transmitted?
The pathogen Chlamydia of serovars L1 to L3, which is responsible for the development of lymphogranuloma venereum, is transmitted through sexual intercourse. It is also possible that a mother suffering from lymphogranuloma venereum infects her newborn child with the disease during birth. The pathogen Chlamydia is a bacterium that is sensitive to dryness and cold and multiplies inside cells.
How can you protect yourself from lymphogranuloma venereum?
You can protect yourself from lymphogranuloma venereum by using a condom. The use of a condom protects equally during vaginal, anal and/or oral sexual intercourse and should be used before especially if the sexual partner is changed frequently .
What are the symptoms of lymphogranuloma venereum?
Typical signs of lymphogranuloma venereum are purulent inflammations of the lymph nodes, which often cause pain and fever. A lymphogranuloma venereum progresses in different phases, whereby sometimes severe complications can occur in the late phase. The respective complaints according to the phase of the disease can be described as follows :
- Stage 1:At the site of infection a painless vesicle develops after an incubation period of about 5 to 21 days, which develops into a superficial ulcer that heals quickly (primary lesion) and is therefore usually not noticed .
- Stage 2:After a further 10 to 30 days, clearly noticeable painful lymph node swellings (so-called bubo) develop, which usually form on one side in the groin and/or thigh area. It is possible for the lymph nodes to burst open, secreting blood and/or pus . The patient feels generally weak and may complain of headache, joint, muscle and/or back pain. There may also be loss of appetite, fever, vomiting and/or nausea. If anal intercourse has been practised, a massive inflammation of the rectal mucosa (proctitis) can also occur, which is noticeable by a mucous and/or bloody discharge, the development of fistulas and/or abscesses and/or cramps.
- If no treatment is given at this stage, the inflammation will heal on its own in a period of about a year, although scars and a constriction of the lymph vessels will develop, which can lead to drainage problems. If left untreated, the disease can lead to severe tissue damage, and some of the chlamydia can also migrate into the lymph nodes of the pelvis and cause the third stage of the disease after a few more years.
- Stage 3 (genitoanorectal syndrome): occurs after about five to ten years of infection and lasts for several years. In this stage, severe inflammation occurs in the anal area and intestines as well as in the external genitals. These inflammations can partially destroy the tissue and contribute to the formation of abscesses, fistulas and pronounced swelling and/or chronic ulcers. In some cases, lymphoedema can also develop or joint inflammation, impairment of the lungs and/or liver can be caused. In rather rare cases, inflammation of the brain and/or heart may occur.
How is lymphogranuloma venereum diagnosed?
In most cases of the disease, lymphogranuloma venereum is diagnosed in the second stage due to the pronounced signs of the disease. An indication of the disease can be the return from an endemic area such as Africa, India, Southeast Asia or the Caribbean, even more so if sexual contact has taken place with a person from the endemic area.
To diagnose the disease, either a smear is taken from the inflamed tissue secretion or from a lymph node and examined in the laboratory. In order to detect the pathogen , various laboratory diagnostic options, such as genetic or cultural pathogen detection methods, can be used to . In some cases, a blood test with antibody detection can also be carried out.
How is lymphogranuloma venereum treated?
A lymphogranuloma venereum is usually treated with an antibiotic. In most cases, the active substance doxycycline is prescribed, which must be taken over a period of three weeks . Therapy with macrolides and/or tetracyclines is also possible .
If the disease is diagnosed at an early stage , it heals quickly without any secondary damage. Depending on the type of inflammatory swelling of the lymph nodes and/or fistulas, surgical removal of these may be necessary. If the disease has only been diagnosed in the third stage, the patient must be treated with long-term antibiotic therapy. If lymphogranuloma venereum remains untreated, especially in the late stages, complications such as lymphoedema very often occur. This is a visible and palpable accumulation of fluid in the interstitial space, the so-called interstitium.
What is the aftercare for lymphogranuloma venereum?
After treatment, a so-called follow-up period should take place over a period of at least six months. In addition, it is advisable that the sexual partner also be examined due to the high risk of infection and, if necessary, also undergo treatment.
Obligation to report
Please note that according to the Austrian Sexually Transmitted Diseases Act, lymphogranuloma venereum is subject to limited notification. In Switzerland, too, the laboratory-analytical findings of the disease must be reported by the laboratories according to the Epidemic Diseases Act.
