What is a pheochromocytoma?
A pheochromocytoma is a mostly benign tumour of the adrenal medulla and often occurs only on one side. The tumour is hormonally active and secretes the hormones adrenaline and noradrenaline, which increase blood pressure. A pheochromocytoma can make itself felt through high blood pressure as well as headaches and/or sweating. Usually, an attempt is made to surgically remove the pheochromocytoma.
What causes a pheochromocytoma to develop?
The exact causes of a pheochromocytoma are still unclear. . However, about one third of all pheochromocytomas can be traced back to genetic changes. In particular, hereditary diseases such as Von Hippel-Lindau syndrome, neurofibromatosis type 1 and multiple endocrine neoplasia type 2 (MEN 2) are suspected to play a decisive role in the development of the disease .
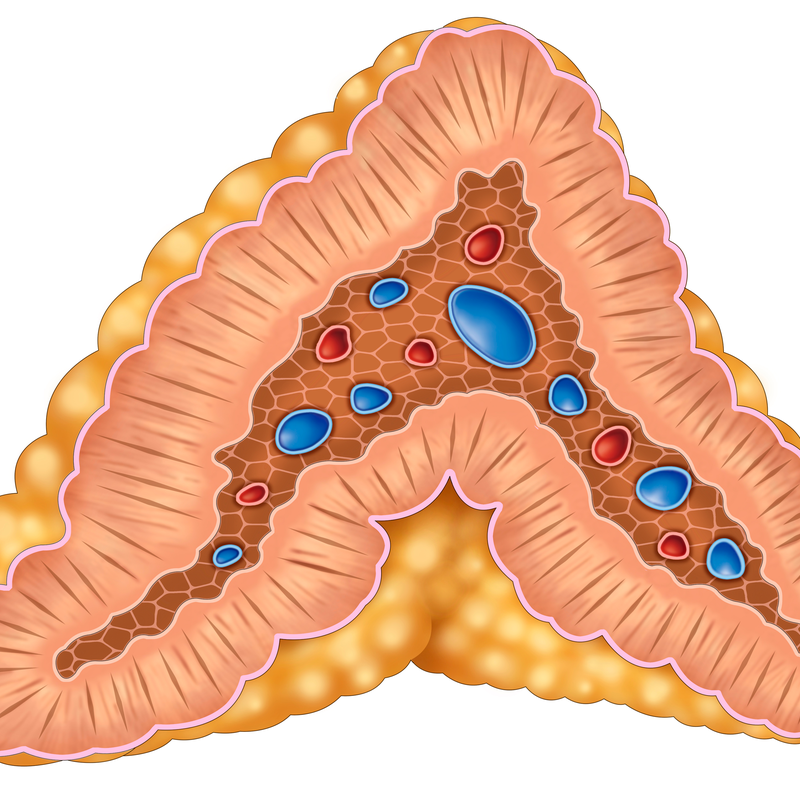
A pheochromocytoma usually originates in the so-called chromaffin cells. These are glandular cells of the adrenal medulla that release the stress hormones adrenaline and noradrenaline and, in rarer cases, the neurotransmitter dopamine . These hormones belong to the catecholamines, which increase the blood pressure. However, there are also rarer forms of pheochromocytoma that develop from chromaffin cells. Chromaffin cells are found outside the adrenal medulla. Doctors refer to these as paragangliomas.
How can a pheochromocytoma be prevented?
Since the causes of pheochromocytoma are still unknown in most cases, there are still no suitable measures to prevent the disease. There are also no corresponding early detection measures for a pheochromocytoma as yet . If you notice that your blood pressure is unusually high, it is advisable to have it checked by a doctor at an early stage. The same applies to cardiac arrhythmias or sudden sweating.
What are the symptoms of a pheochromocytoma?
If a pheochromocytoma releases a large amount of the so-called catecholamines, this leads to a greatly increased blood pressure. In addition, patients complain of the following rather unspecific complaints:
- Headache,
- Sweating and/or perspiration,
- Palpitations, accelerated pulse and even cardiac arrhythmia,
- increased blood sugar level (hyperglycaemia),
- Pallor of the face,
- Dizziness,
- Fatigue,
- unwanted weight loss,
- Nausea,
- Nervousness and/or (inner) restlessness,
- Anxiety and/or panic
How is a pheochromocytoma diagnosed?
A pheochromocytoma can go undetected for a long time. An unusually high blood pressure is sometimes even discovered by chance, for example during an operation. To diagnose a pheochromocytoma, the patient's medical history is first taken. Finally, a physical examination is carried out and the following further findings are collected, which are indispensable for a definite diagnosis:
- Blood and/or urine examination: The degradation products of adrenaline (metanephrine) and noradrenaline (normetanphrine) can be detected in the blood plasma or urine. It should be noted that, for example, alpha blockers, MAO inhibitors and/or tricyclic antidepressants can influence the test results.
- the usual imaging procedures such as an ultrasound examination (sonography), a computer tomography (CT) and/or magnetic resonance imaging (MRI), but also a positron emission tomography (PET) in combination with a CT,
- MIBG scintigraphy: This nuclear medicine method can detect hormone-producing tumours, such as a pheochromocytoma. A MIBG scintigraphy can now also be replaced by a PET.
- Genetic examination: is mainly carried out if there is a suspicion of hereditary causes that could cause the development of a pheochromocytoma . This is the case in about 25 to 40 percent of all cases.
How is a pheochromocytoma treated?
The first choice of treatment for a pheochromocytoma is surgery. This involves removing the adrenal glands along with the tumour (adrenalectomy). In preparation for the operation, patients must take special blood pressure-lowering medication a few days beforehand to prevent the tumour from releasing a large amount of catecholamines. This could have life-threatening consequences for the patient during anaesthesia and surgery .
What is the prognosis for a pheochromocytoma?
The prognosis of a pheochromocytoma depends on several factors. In addition to the question of whether the tumour is benign or malignant, it also depends on whether the disease was diagnosed and treated in time. If the pheochromocytoma could be completely removed by surgery , the prognosis is usually favourable. In most cases the blood pressure normalises after the operation and the symptoms disappear. However, there is a risk that the pheochromocytoma will form again (recurrence). It is therefore extremely important that lifelong annual check-ups take place.
If, on the other hand, a pheochromocytoma remains undetected and untreated, the increased high blood pressure can damage the cardiovascular system in the long term. In addition, the constantly elevated blood pressure can also put other organs at risk.
