What is rhabdomyosarcoma?
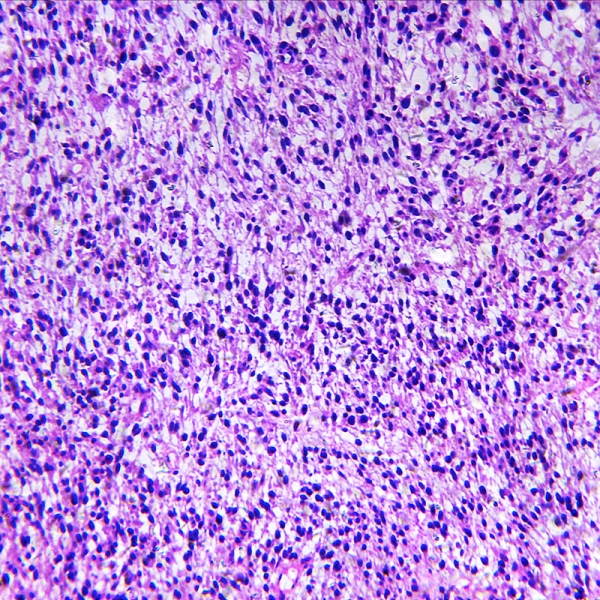
Rhabdomyosarcoma (RMS) is a malignant cancer and is the third most common type of tumour in children outside the central nervous system, occurring disproportionately in children under 7 years of age. The tumour occurs more often in light-skinned children than in dark-skinned children and affects boys slightly more often than girls. The sarcoma arises from embryonic mesenchymal stem cells, i.e. the precursor tissue of the musculature. A rhabdomyosarcoma thus belongs to the group of soft tissue sarcomas and is the most common soft tissue tumour in childhood. It is in turn divided into embryonal and alveolar rhabdomyosarcoma. Rhabdomyosarcoma is diagnosed by computer or magnetic resonance imaging and confirmed by biopsy. Treatment often involves multimodality therapy, i.e. surgical removal of the tumour, followed by radiotherapy and/or chemotherapy.
Where does a rhabdomyosarcoma predominantly form?
In principle, rhabdomyosarcoma can occur anywhere in the body where there is muscle. However, at 35 per cent, it occurs particularly frequently in the head and neck area and here preferably in the nasopharyngeal zone. In addition, about 25 per cent of rhabdomyosarcomas can also develop in the urinary tract or genital organs (urogenital tract). This is especially the case in babies and small children. But rhabdomyosarcoma can also affect the extremities (about 20 per cent) and the trunk (about 20 per cent). At the time of diagnosis, the tumour has already metastasised in 15 to 20 percent of all cases. The lung is the most common site of metastases, along with the bones, bone marrow and lymph nodes. Normally, metastases do not cause any symptoms, especially in the early stages.
What are the symptoms of rhabdomyosarcoma?
The tumour differs in appearance depending on where it occurs. For example, an orbital and nasopharyngeal carcinoma can cause tears and/or eye pain. In addition, a blocked nose, a change in voice and/or discharge of a mucous purulent secretion are also possible symptoms of nasopharyngeal carcinoma.
Genitourinary carcinomas, on the other hand, which usually occur in infants and young children, cause abdominal pain, discomfort when urinating, up to and including blood in the urine and/or a tumour in the abdominal area. Carcinomas of the extremities, on the other hand, manifest themselves as an externally visible tumour that can appear on the arms or legs, for example. The local lymph nodes may also become conspicuous due to swelling.
How is rhabdomyosarcoma diagnosed?
To diagnose a rhabdomyosarcoma, the usual imaging procedures of an ultrasound examination and a computer or magnetic resonance tomography are used first. The latter procedure is more suitable for assessing neck and head tumours. However, for a confirmed diagnosis, the attending physician will also perform a biopsy as well as a bone marrow examination. This is essential to determine the cell type of the tumour and to decide on treatment based on this.
How is a rhabdomysarcoma treated?
Depending on the location of the tumour and its size, rhabdomyosarcoma can in some cases be removed completely surgically immediately after diagnosis. This is especially recommended if the operation is almost risk-free. Sometimes, however, chemotherapy is given first to shrink the tumour and then surgically remove it. Alternatively, radiotherapy may be used.
Children of all categories can be treated with chemotherapy. The drugs most commonly used are actinomycin D (dactinomycin), vincristine, cyclophosphamide, doxorubicin, etoposide and ifosfamide. The newer drugs include topotecan and irinotecan. Radiation therapy, on the other hand, is given to children who still have microscopic residual tumours after surgery. Radiation therapy is therefore primarily reserved for all children with an intermediate and/or high risk.
What is the prognosis for rhabdomyosarcoma?
The prognosis of a rhabdomyosarcoma depends not only on its location but also on the type of tumour and the patient's general state of health. If the tumour has already spread to metastases, the chances of cure decrease accordingly. After weighing all these prognostic factors, the patient can be placed in a low, medium or high risk category. Generally, the survival rate for children in the low-risk category is less than 90 per cent, while that of children in the high-risk category is more than 50 per cent.
Especially in the head and neck area, rhabdomysarcoma often returns after treatment. In most cases, the tumour then forms again at least in the vicinity of the original tumour site, as scientists reported in the scientific journal "European Journal of Cancer". Within their study, they referred to the data of 165 patients who suffered from a localised rhabdomyosarcoma in the head and neck area. The age of all patients at first diagnosis ranged from a few months to 25 years. In most cases, the rhabdomyosarcoma had developed on the cheek, chin or nostrils. Most of the tumour tissue had characteristics that indicated a rather unfavourable prognosis. Most of the patients were treated with radiotherapy and/or surgery.
In about a quarter of the patients, the tumour regressed within five years after diagnosis. The tumour often appeared in the oral cavity, in the parotid gland, the chin, the cheek or the nostril. In most cases, the tumour recurred at least in the vicinity of the first tumour site. The 5-year survival rate was 85 percent. In three quarters of all patients, the cancer had not returned. The location of the original tumour had no influence on whether the cancer returned or not. The authors of the study concluded that the general prognosis for children with rhabdomyosarcoma of the head and neck is rather good.
