What is vulvar cancer?
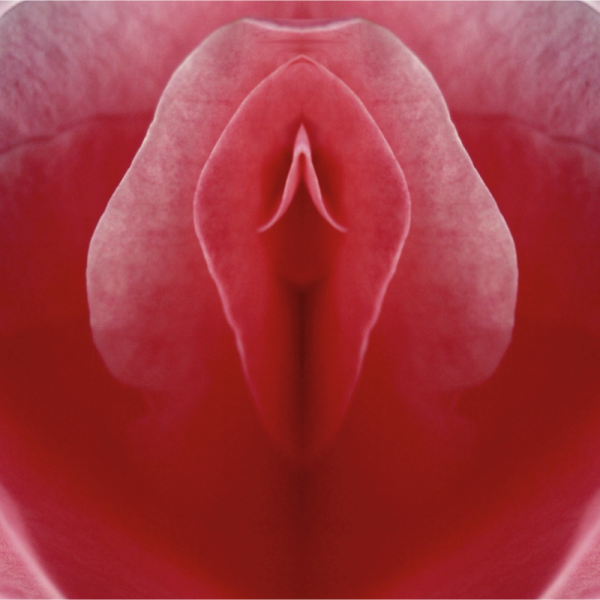
Vulvar carcinoma is a rare malignant cancer of the external female genitalia. Vulvar cancer usually originates from the squamous epithelium of the skin, but in rare cases it can also originate from the Bartholinian glands, which are located at the entrance to the vagina or at the clitoris or urethra. In the past, older women were more likely to develop vulvar carcinoma, but nowadays more and more young women are developing the disease. Human papilloma viruses (HPV) can often play a decisive role in the development of vulvar carcinoma. Vulvar cancer is the fourth most common cancer of the female genital organs. Where does vulvar cancer develop?
Vulvar cancer can develop anywhere in a woman's pubic area. However, it usually develops in the area of the front vulva, and can therefore be located between the labia minora, i.e. in the area between the clitoris and the urethra, or on the clitoris itself. In addition, some vulvar cancer may be found on the side of the labia majora, i.e. close to the bowel outlet (perineum) or at the posterior vaginal entrance.
What are the different types of vulvar carcinoma?
Doctors distinguish between the following types of vulvar carcinoma:
- mild preliminary vulvar carcinoma: is usually caused by an infection with the human papillomavirus (HPV),
- invasive vulvar carcinoma: is characterised by tumour cells that have already grown further into the surrounding tissue,
What are the symptoms of vulvar cancer?
Vulvar carcinoma initially manifests itself through rather unspecific symptoms such as a burning sensation when urinating, itching or a small skin lesion. If there are visible skin changes, these can indicate a preliminary stage of vulvar cancer. If the adjacent hollow organs such as the bowel or bladder outlet or the vagina are affected by vulvar cancer, there may also be pain during sexual intercourse or urination, but also bleeding.
How can vulvar cancer be prevented?
So far, there is no screening test to diagnose the disease in advance. However, as part of the annual gynaecological screening, the cervix is examined and a Pap smear is taken. For this reason, it is advisable to attend regular screening examinations. Since human papilloma viruses (HPV) can often contribute to the development of vulvar cancer, HPV vaccination can be useful.
How is vulvar cancer diagnosed?
Vulvar cancer can be diagnosed by chance, for example during a gynaecological check-up. If it is found during this examination that the tissue in the vulva area is altered, a detailed examination will take place. If carcinoma is suspected, a tissue sample (biopsy) will be taken and analysed in the laboratory.
If it is determined at the time of the examination that the disease is already more advanced, because the carcinoma has already extended beyond the mucous membrane of the vulva, for example, the usual imaging procedures are used. In addition to an ultrasound examination, the gynaecologist can also carry out a computer tomography (CT) or magnetic resonance imaging (MRI). In addition, the neighbouring organs such as the bladder and rectum can also be mirrored to assess the stage of the disease. It is also important to find out if the lymph nodes are affected. This can be done by palpating the lymph nodes or by doing a CT or MRI scan.
How is vulvar cancer treated?
Treatment is usually not immediately necessary for mild precancerous lesions of the vulva. A gynaecologist should check the affected areas of skin regularly and the patient should watch out for any new symptoms. If it is an invasive vulvar carcinoma, however, the doctor will usually cause the tumour to be removed surgically as completely as possible. The vulva is then reconstructed using plastic procedures. If the tumour is particularly large, combined radiation chemotherapy may also be given before surgery to shrink the carcinoma.
If the vulvar carcinoma has already spread to other organs, a cure is often no longer possible. The patient's symptoms should be alleviated first and foremost. If necessary, chemotherapy can be administered.
What is the aftercare for vulvar cancer?
In the first five years after the operation, follow-up examinations take place every year for several years. After the sixth year, one follow-up examination per year is sufficient. During the follow-up examinations, the patient is first examined physically. This is followed by an imaging examination. If abnormalities are discovered, the gynaecologist takes a tissue sample (biopsy) of the suspicious tissue.
Further targeted supportive measures (supportive therapy) can help to alleviate other possible side effects. These include, for example, a change in the condition of the vulva, vaginal constriction, inflammation of the mucous membranes and/or lymphoedema.
What is the prognosis for vulvar cancer?
The prognosis depends on various factors. In addition to the size of the vulvar carcinoma, the depth to which the tumour has already grown into the underlying tissue is also decisive. The chances of cure also depend on whether the lymph nodes in the groin and/or pelvis are affected. If the lymph nodes are affected, the prognosis is much worse. If the cancer has already metastasised to other organs, which is usually the case at an advanced stage or with a recurring tumour, vulvar cancer is incurable.
After successful treatment, many patients complain that they can no longer control their urine and/or stool excretion properly. In this case, doctors speak of incontinence, which can occur mainly because the vulva is anatomically close to the urinary bladder and the intestines. Doctors therefore recommend targeted pelvic floor training, which can be carried out by a physiotherapist, for example.
